Health
World Cancer Day 2025: Ditch These 10 Habits to Lower Your Cancer Risk
Contents
Understanding Cancer Risks
Cancer is a complex group of diseases characterized by the uncontrolled growth and spread of abnormal cells in the body. It remains one of the leading causes of morbidity and mortality worldwide, with the World Health Organization estimating that nearly 10 million deaths were attributed to cancer in 2020 alone. As the global population ages and lifestyle choices evolve, the prevalence of various types of cancer is expected to rise, making it imperative for individuals to understand cancer risk factors.
Understanding cancer risks is crucial for implementing effective prevention strategies. Numerous studies have identified several lifestyle factors that contribute to the development of cancer. Among these, tobacco use, poor diet, physical inactivity, and excessive alcohol consumption have been consistently linked to increased cancer incidence. Moreover, environmental exposures such as radiation, pollution, and certain chemicals further augment the risk. Awareness of these factors not only empowers individuals to make informed choices but also fosters a proactive approach to health management.
By recognizing how everyday habits can influence cancer risk, individuals can adopt healthier lifestyles that may significantly lower their chances of developing the disease. For instance, a balanced diet rich in fruits, vegetables, and whole grains has been associated with a reduced risk of various cancers. Additionally, regular physical activity is a vital element in maintaining a healthy weight, which can also play a role in minimizing cancer risk. Understanding these connections encourages individuals to scrutinize their habits critically and identify areas for improvement.
As we move forward to explore specific habits that can be altered to mitigate cancer risk, it is essential to remember that while some risk factors, such as genetics, cannot be changed, many others can be modified through lifestyle choices. This understanding lays the groundwork for making impactful decisions that could lead to better health outcomes. By evaluating and adjusting these habits, individuals stand a greater chance of reducing their vulnerability to cancer.
The Importance of World Cancer Day
World Cancer Day, observed annually on February 4th, serves as a vital platform for raising awareness about cancer prevention, detection, and treatment. Established in 2000 by the Union for International Cancer Control (UICC), this global initiative aims to unite individuals and organizations worldwide in the fight against cancer, emphasizing that everyone can play a role in reducing the impact of this disease.
The significance of World Cancer Day lies not only in its ability to raise awareness but also in its role as a catalyst for change. By encouraging individuals, communities, and governments to actively participate in various activities centered around prevention, the day seeks to educate the public about the importance of healthy lifestyle choices that can decrease risk. Campaigns and initiatives undertaken on this day reflect a commitment to making a global impact on cancer care, screening, and research.
Past World Cancer Day campaigns have showcased remarkable successes in fostering increased public awareness and funding for cancer research. For instance, initiatives such as the “I Am and I Will” campaign emphasize personal commitments to action, engaging individuals in a collective movement aimed at reducing stigma around the disease and promoting proactive measures in cancer care. Global partnerships with healthcare organizations, governments, and non-profits have also contributed to substantial advancements in cancer treatment and prevention strategies.
Moreover, It plays a critical role in empowering patients and caregivers by providing them with resources and information regarding available treatment options. It highlights the necessity of early detection and timely intervention, which are paramount for improving survival rates. Overall, this not only raises awareness about this but also inspires a collective effort towards fostering a healthier global community focused on combating through shared knowledge and proactive strategies.
Habit 1: Smoking and Tobacco Use
Smoking and tobacco use are leading contributors to cancer risk worldwide, with substantial evidence linking them to various forms of the disease. Research indicates that smoking is responsible for approximately 22% of deaths globally, affecting both smokers and non-smokers through secondhand exposure. The carcinogenic properties of tobacco stem from the chemicals released when tobacco is burned, which can cause mutations in cellular DNA, ultimately leading to tumor growth. It is the most frequently diagnosed cancer among smokers, but tobacco use is also associated with cancers of the throat, mouth, esophagus, bladder, and pancreas, among others.
The health implications of smoking extend well beyond this . Smokers often experience chronic respiratory issues, heart disease, and a diminished immune response, increasing vulnerability to various illnesses. The World Health Organization (WHO) emphasizes that tobacco cessation is the single most effective method for reducing cancer risk. In fact, individuals who quit smoking can significantly decrease their likelihood of developing smoking-related cancers over time, with the risk of lung cancer potentially halving after ten years of abstinence.
Fortunately, several resources are available to support individuals in their journey to quit smoking. This can include behavioral therapies, counseling, and various aids such as nicotine replacement therapy (NRT) or prescription medications designed to reduce cravings. Additionally, many health organizations have developed cessation programs that provide education on coping strategies and ways to avoid triggers. By adopting healthier alternatives, such as engaging in physical activity or practicing mindfulness, individuals can better manage withdrawal symptoms and reduce the likelihood of relapse.
Addressing smoking and tobacco use is a crucial step in lowering risk. Undertaking efforts to quit will not only provide immediate health benefits but also contribute to long-term cancer prevention, ultimately fostering a healthier future for individuals and communities alike.
Habit 2: Poor Dietary Choices
Diet plays a critical role in influencing an individual’s risk of developing various forms of cancer. In recent studies, researchers have highlighted that poor dietary choices, particularly those high in processed foods, sugars, and unhealthy fats, can significantly elevate the likelihood of certain cancers. For instance, diets rich in red and processed meats are associated with an increased risk of colorectal cancer. Additionally, frequent consumption of sugary beverages and high-calorie foods can lead to obesity, which is a well-established risk factor for several types of cancer, including breast, prostate, and endometrial cancers.
Another concerning trend is the lack of fruits and vegetables in the average diet. A deficiency in these nutrient-dense foods can deprive the body of essential vitamins, minerals, and antioxidants that play a pivotal role in maintaining cellular health and combating cancer. Fruits and vegetables contain phytochemicals that have been shown to reduce inflammation and promote apoptosis in precancerous cells, mitigating development.
To lower the risk through dietary modifications, individuals should emphasize the intake of whole grains, lean proteins, and healthy fats. Incorporating a variety of colorful fruits and vegetables into daily meals not only enhances the nutritional profile of one’s diet but also introduces a range of protective compounds against cancer. Foods such as berries, leafy greens, and cruciferous vegetables like broccoli and kale are particularly beneficial. Furthermore, adopting cooking methods like steaming, roasting, or grilling can help in reducing the harmful effects associated with frying or heavily processing foods.
In recognizing the link between dietary choices and their risk, it is essential for individuals to adopt a balanced and mindful approach to eating that prioritizes whole and unprocessed foods. By making conscious choices, one can significantly contribute to prevention efforts, ultimately promoting better health and well-being.
Habit 3: Physical Inactivity
Physical inactivity is a significant contributor to various health issues, including an increased risk of cancer. According to research from organizations such as the World Health Organization, sedentary lifestyles are linked to various types of cancer, including breast, colon, and endometrial . The statistics are compelling; individuals who engage in minimal physical activity can find themselves at a 20-30% higher risk of developing certain compared to their more active counterparts. This correlation highlights the importance of integrating regular exercise into daily routines.
Regular physical activity not only aids in weight management—a vital factor in reducing cancer risk—but also enhances overall physical and mental well-being. Exercise has been shown to improve immune function, reduce inflammation, and help regulate hormones, all of which are critical in lowering the potential for cancer development. Engaging in just 150 minutes of moderate aerobic exercise or 75 minutes of vigorous exercise weekly can yield significant health benefits and aid in \ risk reduction.
Incorporating physical activity into daily life doesn’t have to be overwhelming. Simple strategies can make a substantial difference. For instance, opt for walking or cycling instead of driving for short distances. Incorporating short bursts of activity throughout the day, such as taking the stairs instead of the elevator or performing quick stretching exercises during breaks, can contribute to increased energy expenditure. Joining a community sports team or enrolling in a fitness class can also provide social support and enhance motivation to stay active.
Ultimately, adopting an active lifestyle can serve as a powerful tool in combating cancer risk. By prioritizing physical activity, individuals not only improve their quality of life but also contribute to their long-term health, making significant strides toward reducing the prevalence of cancer in society.
Habit 4: Excessive Alcohol Consumption
Excessive alcohol consumption has been identified as a significant risk factor for various types of cancer. Research indicates that alcohol may contribute to the development of at least seven different cancers, including breast, liver, colorectal, and esophageal cancer. The relationship between alcohol use and their risk is complex, as the metabolism of alcohol in the body can produce carcinogenic compounds that damage DNA and disrupt hormonal balance. Moreover, alcohol consumption may exacerbate the harmful effects of other cancer risk factors, such as smoking.
The strength of the association between alcohol intake and cancer varies by type. For instance, studies show that consuming more than one drink per day for women and two drinks for men increases the risk of breast cancer. Additionally, high alcohol intake has a pronounced effect on liver, particularly in individuals with pre-existing liver conditions or chronic hepatitis infections. As a result, health professionals advocate for moderation in drinking habits as a key strategy to mitigate risk.
Reducing alcohol intake can lead to numerous health benefits beyond prevention. These benefits include improved liver function, better cardiovascular health, and enhanced cognitive abilities. Individuals seeking alternatives to traditional alcoholic beverages may find success in exploring non-alcoholic options, such as flavored sparkling water, herbal teas, or mocktails, which can provide the social enjoyment of drinking without the associated health risks.
In terms of overall health and well-being, it is wise to consider minimizing alcohol consumption. By doing so, individuals not only lower their risk but also embrace a more health-conscious lifestyle. Prioritizing moderation can be a significant step toward long-term health and reducing the likelihood of developing alcohol-related health issues.
Habit 5: Ignoring Sun Safety
UV exposure poses significant risks to skin health, with a notable link to various forms of skin , including melanoma, which is the most lethal type. Overexposure to ultraviolet rays, particularly during peak sun hours, increases the likelihood of severe sunburns. These sunburns can cause immediate discomfort and damage to the skin, setting the stage for long-term health consequences, including cancer development. Therefore, understanding the significance of sun safety is essential for reducing risk.
Implementing sun safety measures is crucial for protecting skin from harmful UV rays. One of the most effective practices is the regular application of broad-spectrum sunscreen with a high SPF rating. It should be applied generously and frequently, particularly after swimming or sweating, to ensure optimal protection. Additionally, wearing protective clothing, such as long-sleeved shirts, wide-brimmed hats, and UV-blocking sunglasses, can significantly reduce skin exposure to harmful rays.
Seeking shade during the sun’s peak intensity, typically between 10 a.m. and 4 p.m., is also recommended. This can help minimize direct UV exposure and subsequently lower the risk of skin damage. Moreover, regular skin checks at home can play a crucial role in early detection of abnormalities. Monitoring moles or skin changes allows individuals to seek timely medical advice, should any suspicious characteristics arise.
Incorporating these sun safety practices into daily routines is vital for safeguarding against the dangers associated with UV exposure. By making conscious efforts to prioritize skin health and actively engage in preventive measures, individuals can significantly reduce their risk and maintain healthier skin over time.
Habit 6: Neglecting Regular Medical Screenings
Regular medical screenings play a crucial role in the early detection of , significantly impacting treatment outcomes and survival rates. These screenings allow for the identification of potential cancerous changes before symptoms become apparent. As a proactive measure, individuals are encouraged to adhere to recommended guidelines for medical screenings, which vary based on age, gender, and personal health history.
For instance, women are advised to begin regular mammograms to screen for breast cancer at the age of 40, or earlier if they have a high risk of breast cancer. Similarly, cervical cancer screenings through Pap smears should start at age 21, with follow-up screenings occurring at intervals based on age and previous results. Men, on the other hand, should discuss prostate screening options with their healthcare providers when they reach the age of 50, or at 45 for those with a family history of the disease.
Colorectal cancer screenings are recommended for both men and women beginning at age 45. These screenings can include colonoscopies or home stool tests, which can respectively detect and help prevent the onset of this type of cancer. Additionally, skin examinations for suspicious moles or changes in the skin are essential for early identification of skin cancer, which is becoming increasingly prevalent.
Also read : Rising Norovirus Cases in the US: Understanding Spread and Precautions
Beyond age and gender-specific recommendations, individuals with a family history of certain should remain vigilant about their screening schedules. Genetic counseling and testing may be beneficial in these cases, guiding the choice of proactive measures. Engaging in regular medical screenings fosters a culture of health awareness, allowing individuals to take informed steps towards reducing their cancer risk.
By prioritizing regular health check-ups and screenings, individuals can be actively involved in protecting their well-being, ultimately lowering the risk of developing cancer through early intervention.
Habit 7: Chronic Stress and Poor Mental Health
Chronic stress has emerged as a significant factor that can influence an individual’s overall health and may increase the risk of developing cancer. Prolonged exposure to stress can lead to the release of stress hormones, such as cortisol, which in high levels, can contribute to inflammation and weaken the immune system. This weakened state can impair the body’s ability to detect and eliminate cancer cells, thereby heightening the likelihood of tumor proliferation. Furthermore, stress often leads to unhealthy coping mechanisms, such as poor dietary choices, lack of physical activity, and substance abuse, all of which can additionally contribute to an increased risk.
To mitigate the impact of chronic stress on health, it is essential to implement effective stress management techniques. Mindfulness practices, such as meditation and yoga, have shown promise in alleviating stress and fostering a sense of calm. These practices can promote emotional well-being and strengthen mental resilience. Engaging in regular physical activities, such as walking, cycling, or swimming, can further help to reduce stress levels while enhancing overall fitness. Additionally, maintaining a balanced diet rich in fruits, vegetables, whole grains, and healthy fats can provide the body with necessary nutrients that support emotional health and bolster the immune system.
Furthermore, establishing a strong support system through social engagements and talking to friends or family can significantly improve one’s mental health. Seeking professional help from therapists or counselors can provide individuals with coping strategies to manage stress effectively. Maintaining a positive mindset and addressing issues before they escalate into chronic stress can create a proactive approach to health management. By adopting these strategies, individuals can not only lower their risk but also enhance their quality of life, making mental health a critical aspect of cancer prevention efforts.
Summary: Taking Action Towards a Cancer-Free Future
As we reflect on the various habits outlined in this article, it becomes clear that individual choices play a significant role in shaping our overall health and well-being. Each habit discussed contributes to a cumulative risk, enhancing the likelihood of developing cancer over time. By recognizing and addressing these detrimental habits, we can significantly lower our cancer risk and pave the way toward a healthier future.
Awareness is the first step toward prevention, and it is vital that we take a comprehensive approach to combating Making informed decisions about our lifestyle, such as adopting a balanced diet, engaging in regular physical activity, and avoiding harmful substances, can have a profound impact not just on our health, but also on those around us. It is essential to consider how these habits affect our families, friends, and communities; promoting a culture of health can lead to collective action against cancer.
Moreover, education is a powerful tool in the quest for prevention. There are numerous resources available to deepen your understanding of risks and prevention strategies. Organizations dedicated to their research and advocacy provide helpful information on lifestyle changes, support groups, and preventive screenings. Taking advantage of these resources not only empowers individuals to make better choices but also fosters a community of support and awareness. This communal approach can effectively combat cancer and reduce its prevalence.
Breaking News
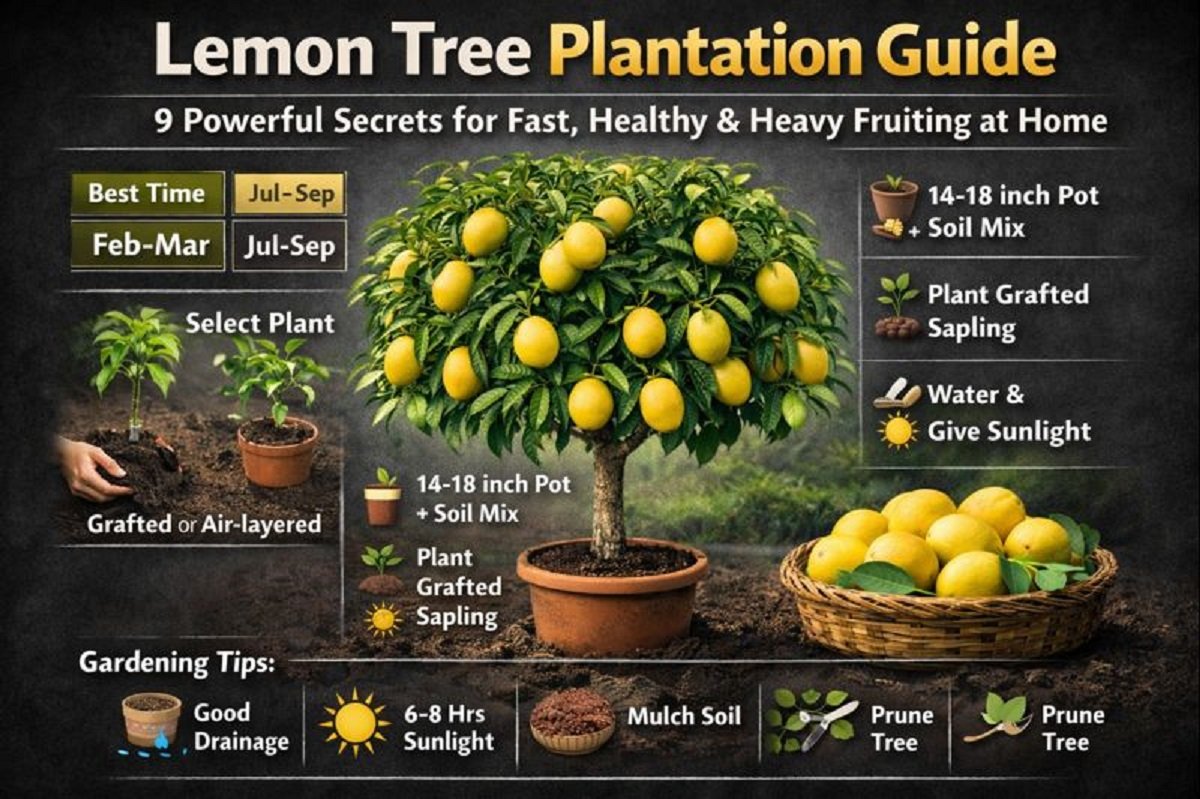
Lemon Tree Plantation Guide-
Contents
Jaipur, Jan.05,2026:Lemon Tree Plantation Guide is emerging as one of the most searched home-gardening topics across India as urban households increasingly turn toward terrace gardening and organic fruit production. Lemon, known for its year-round utility, medicinal value, and high vitamin-C content, is among the easiest fruit trees to grow at home.
This Lemon Tree Plantation Guide explains when, where, and how to plant a lemon tree in pots or soil using scientifically proven methods followed by horticulture experts.
Why Lemon Tree Plantation Is Trending in 2026
According to gardening experts and agricultural advisories, lemon trees are
- Fast-growing
- Suitable for pots
- Productive within 12–18 months
- Ideal for Indian climate
With rising food adulteration concerns, the Lemon Tree Plantation Guide has become a must-read for health-conscious families.
Best Time to Plant
Choosing the correct planting season is critical.
Best Months
- February–March
- July–September
These periods provide optimal temperature and humidity, ensuring faster root establishment and healthy growth.
Ideal Soil & Pot Selection
Soil Requirements
- Well-drained sandy loam soil
- Rich in organic matter
- Slightly acidic to neutral pH
Soil Mix
- 40% cow dung manure or vermicompost
- 10% river sand
- 50% garden soil
Good drainage is a non-negotiable rule in every professional Lemon Tree Plantation Guide.
Choosing the Right Plant
Always buy
- Grafted (कलम किया हुआ) or
- Air-layered lemon plant
Why
- Faster fruiting
- Strong disease resistance
- Uniform fruit quality
Experts from horticulture departments recommend grafted citrus plants for home gardens.
Step-by-Step Plantation Method
Step 1: Pot Preparation
- Use a 14–18 inch pot or grow bag
- Ensure multiple drainage holes
Step 2: Planting the Lemon Tree
- Remove plant gently from nursery bag
- Plant at the same depth as earlier
- Keep the grafting joint above soil level
- Press soil lightly around the roots
Step 3: Initial Watering
- Water immediately after planting
- Keep soil moist, not waterlogged
This phase is crucial in the Lemon Tree Plantation Guide.
Watering Schedule
- Summer: Every 2–3 days
- Winter: Once a week
- Rainy season: Only if soil is dry
Excess water can cause root rot — the most common lemon plant killer.
Sunlight Requirement
Lemon trees need
- 6–8 hours of direct sunlight daily
Balcony, terrace, or open garden locations work best.
Fertilizer & Nutrition Management
Apply organic fertilizers every 1–2 months
- Vermicompost
- Mustard cake solution
- Banana peel compost
- Neem cake
Healthy nutrition ensures continuous flowering and fruiting as explained in this Lemon Tree Plantation Guide.
Pruning & Growth Control Techniques
- Remove dead or diseased branches
- Light pruning promotes new shoots
- Best time: After harvesting
Pruning keeps the lemon tree compact and productive.
Common Problems and Their Solutions
Flower Drop
Causes
- Lack of moisture
- Nutrient deficiency
Solution
- Maintain soil moisture
- Apply organic fertilizer
Yellow Leaves
Cause
- Overwatering or poor drainage
Solution
- Improve soil aeration
Benefits of Growing Lemon Tree at Home
- Fresh chemical-free lemons
- Saves money
- Improves air quality
- Enhances home aesthetics
- Year-round harvesting
Expert Tips for Faster Fruiting
- Mulch soil to retain moisture
- Use Epsom salt occasionally
- Avoid chemical fertilizers
- Rotate pot for uniform sunlight
This Lemon Tree Plantation Guide proves that growing lemons at home is not complicated if the right techniques are followed. With proper timing, soil preparation, sunlight, and organic care, your lemon plant can produce healthy fruits for years.
Breaking News
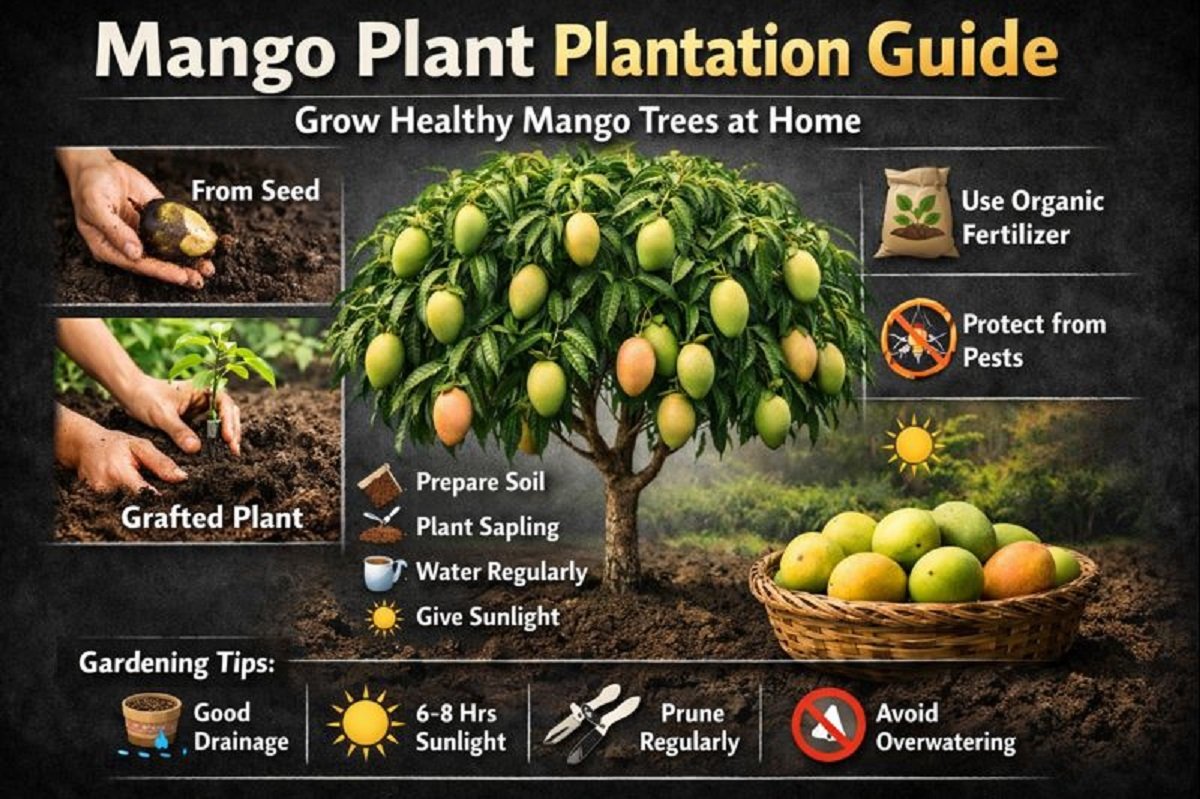
Mango Plant Plantation Guide-
Contents
Jaipur,Jan.05,2026:Mango Plant Plantation Guide is becoming one of the most searched gardening topics in India as more people turn towards home gardening, organic fruits, and sustainable living. Mango, known as the King of Fruits, holds deep cultural, nutritional, and economic value.
Whether you live in a house with a backyard or an apartment with a terrace, this Mango Plant Plantation Guide will help you grow a healthy mango tree using either a seed (गुठली) or a nursery-grown grafted plant.
Why Mango Plantation Is Gaining Popularity
The rising demand for chemical-free fruits and the joy of growing food at home have made mango plantation a trending topic. According to horticulture experts and agricultural advisories, mango trees are hardy, long-living, and highly rewarding when planted correctly.
This Mango Plant Plantation Guide explains simple yet powerful methods that even beginners can follow.
Best Climate & Soil
- Climate: Tropical to subtropical
- Temperature: 24°C – 35°C
- Soil Type: Well-drained loamy or sandy loam
- Soil pH: 5.5 – 7.5
Good drainage is critical. Waterlogged soil can damage mango roots permanently.
Mango Plant Plantation Guide Using Seed (गुठली से पौधा लगाना)
Growing mango from seed is economical and educational, though it takes more time to bear fruit.
Step 1: Seed Preparation
- Wash the mango stone thoroughly
- Dry it for 1–2 days
- Carefully break the outer shell
- Extract the inner seed
- Wrap it in a moist cloth for germination
This step is crucial in the Mango Plant Plantation Guide.
Step 2: Pot & Soil Preparation
- Use a 12–18 inch pot with drainage holes
- Mix:
- Garden soil
- Compost
- Well-decomposed cow dung manure
Healthy soil is the foundation of successful mango growth.
Step 3: Planting the Seed
- Plant the germinated seed 2 inches deep
- Cover lightly with soil
- Water gently
Step 4: Early Care
- Keep the pot in partial shade
- Maintain moisture, not excess water
- Once the plant grows stronger, shift it to a 45 cm deep pot or garden soil
This stage defines success in the Mango Plant Plantation Guide.
Mango Plant Plantation Guide Using Nursery (Grafted) Plant
For faster fruiting, experts recommend grafted plants.
Step 1: Selecting the Right Plant
- Choose a healthy, disease-free grafted mango plant
- Preferred varieties: Alphonso, Dasheri, Langra, Kesar
Step 2: Pit Preparation
- Dig a pit of 1x1x1 feet
- Best done during summer
- Mix excavated soil with:
- Compost
- Cow dung manure
- Trichoderma (bio-fungicide)
Step 3: Plantation
- Place plant gently without damaging roots
- Fill pit with prepared soil
- Press soil lightly around base
Step 4: Watering & Shade
- Water immediately
- Provide shade for initial days
- Gradually expose to sunlight
This method is widely recommended in professional Mango Plant Plantation Guide manuals.
Watering Schedule
- Initial stage: Water every 2–3 days
- Established plants: Once a week
- Avoid waterlogging
Overwatering is one of the biggest mistakes in mango cultivation.
Sunlight & Location
- Young plants need protection from harsh sunlight
- Mature mango trees need 6–8 hours of direct sunlight daily
Sun exposure directly affects flowering and fruit quality.
Fertilizer & Nutrition Management
Apply organic manure during
- July–August
- September
Recommended nutrients:
- Compost
- Vermicompost
- Neem cake
Balanced nutrition is a core principle of any Mango Plant Plantation Guide.
Protection From Pests & Animals
- Use fencing or bamboo support
- Protect young plants from goats and cattle
- Apply neem oil spray for pest control
Common Mistakes to Avoid
- Excess watering
- Poor drainage
- Ignoring sunlight needs
- Planting in very small containers
Avoiding these mistakes ensures success with this Mango Plant Plantation Guide.
Benefits of Growing Mango at Home
- Chemical-free fruits
- Long-term investment
- Environmental benefits
- Shade and greenery
- Emotional satisfaction
Expert Gardening Tips
- Mulch soil to retain moisture
- Prune lightly after 2–3 years
- Use organic pesticides only
This Mango Plant Plantation Guide is designed to help beginners and gardening enthusiasts grow mango trees successfully at home. With patience, proper care, and organic practices, your mango tree will thrive for decades and reward you with delicious fruits.
Breaking News
Chyawanprash Health Benefits-

Contents
Jaipur,Jan.02,2026:Chyawanprash Health Benefits have made this ancient Ayurvedic formulation an inseparable part of Indian households. From children to the elderly, millions rely on it daily to strengthen immunity, enhance energy levels, and protect the body from seasonal illnesses.
In today’s world of rising pollution, frequent infections, and stressful lifestyles, people are actively searching for natural and preventive health solutions. This is where Dabur Chyawanprash Health Benefits stand out—offering a time-tested, research-backed approach to holistic wellness.
A Timeless Ayurvedic Rasayana
Chyawanprash is one of the oldest known Ayurvedic Rasayana (rejuvenation tonic), mentioned in classical texts like the Charaka Samhita and Rigveda. Traditionally prepared to restore youthfulness and vitality, it was originally formulated for sage Chyawan to regain strength and longevity.
Ayurvedic scholars describe it as an “Ageless Wonder” due to its ability to nourish body tissues, strengthen immunity, and slow down ageing.
Learn more about Rasayana therapy from the Ministry of AYUSH
Health Benefits Backed by Ayurveda & Science
Unlike many modern supplements, Dabur Chyawanprash Health Benefits are rooted in both ancient wisdom and modern scientific validation. Dabur has combined centuries-old Ayurvedic knowledge with contemporary research, quality control, and innovation.
Each spoon contains a powerful blend of Amla (Indian Gooseberry), natural antioxidants, essential minerals, and over 40 Ayurvedic herbs.
The Core of Chyawanprash Health Benefits
One of the most trusted Dabur Chyawanprash Health Benefits is its powerful effect on immunity.
How It Works
- Enhances Immunoglobulin G (IgG) and IgM, which protect against infections
- Helps regulate IgE, reducing allergic reactions
- Lowers histamine levels, easing respiratory and seasonal allergies
Scientific studies indicate that regular consumption improves the body’s immune response against pathogens.
How Chyawanprash Boosts Energy, Stamina, and Vitality
Low energy and fatigue are common problems across age groups. Dabur Chyawanprash Health Benefits include natural energy enhancement without artificial stimulants.
Key Advantages
- Improves oxygen utilization
- Enhances metabolic efficiency
- Supports muscle and tissue nourishment
- Reduces tiredness and weakness
This makes it ideal for students, working professionals, athletes, and senior citizens.
The Ayurvedic Advantage
According to Ayurveda, good health depends on the balance of Vata, Pitta, and Kapha doshas.
Dabur Chyawanprash Health Benefits include
- Calming excess Vata (reduces weakness and anxiety)
- Regulating Pitta (supports digestion and metabolism)
- Strengthening Kapha (boosts immunity and endurance)
This tri-dosha balance ensures overall physical and mental harmony.
Anti-Ageing and Antioxidant Properties Explained
Ageing begins at the cellular level. Dabur Chyawanprash Health Benefits include protection against oxidative stress caused by free radicals.
Antioxidant Power
- High polyphenols and gallic acid from Amla
- Flavonoids and tannins for cellular repair
- Supports skin health, memory, and organ function
These compounds slow down premature ageing and promote youthful vitality.
The Power of Amla and 40+ Herbs in Dabur Chyawanprash
Amla forms the backbone of Dabur Chyawanprash, providing natural Vitamin C in its most stable form.
Key Ingredients Include
- Amla – Immunity and antioxidant powerhouse
- Pippali – Respiratory support
- Ashwagandha – Stress relief and stamina
- Giloy – Detox and immune modulation
- Cow Ghee & Sesame Oil – Nutrient absorption enhancers
Together, they amplify Dabur Chyawanprash Health Benefits manifold.
Scientific Research Supporting Chyawanprash Health Benefits
Experimental studies reveal that Chyawanprash
- Reduces allergic responses
- Lowers serum IgE levels
- Suppresses histamine release
- Improves long-term immune memory
Such findings validate Ayurveda through modern biomedical research.
Allergy Protection and Respiratory Wellness
Seasonal cough, asthma, and breathing issues worsen in winter. Chyawanprash Health Benefits extend to respiratory health by:
- Strengthening lung tissues
- Reducing inflammation
- Improving airflow and oxygen exchange
It acts as a protective shield against pollution-related respiratory problems.
Why Chyawanprash Is Different From Other Supplements
Unlike synthetic immunity boosters, Dabur Chyawanprash
- Is natural and preservative-free
- Works holistically, not symptomatically
- Is safe for long-term daily use
- Is backed by over 135 years of Ayurvedic expertise
This makes Dabur Chyawanprash Health Benefits truly sustainable.
How to Consume Chyawanprash for Maximum Health Benefits
Recommended Dosage
- Adults: 1–2 teaspoons daily
- Children: ½–1 teaspoon daily
Consume with warm milk or water for better absorption.
Who Should Take Chyawanprash
- Children with low immunity
- Adults facing fatigue and stress
- Elderly individuals
- People prone to allergies
- Anyone seeking natural wellness
Chyawanprash in Modern Indian Lifestyle
In today’s fast-paced life, Dabur Chyawanprash Health Benefits offer a simple daily ritual for long-term health—bridging ancient wisdom with modern living.
Why Chyawanprash Remains India’s Daily Health Shield
Chyawanprash Health Benefits go far beyond immunity. They represent India’s holistic approach to health—natural, preventive, and deeply rooted in tradition.
From boosting energy and protecting against diseases to slowing ageing and enhancing vitality, Chyawanprash continues to be a trusted wellness companion for every Indian household.
Breaking News
Fat Loss Drugs in India are gaining massive attention after Ozempic’s launch-

Contents
Jaipur, Dec.17,2025:Fat Loss Drugs in India have become one of the most discussed topics in the health and pharmaceutical space after the official launch of Ozempic by Danish drugmaker Novo Nordisk. Originally developed to treat Type-2 diabetes, this injectable medicine is now being widely talked about for its remarkable weight loss effects.
From celebrities to medical experts, everyone seems to be debating whether these drugs are a breakthrough solution for obesity or a risky shortcut. With India facing a twin epidemic of diabetes and obesity, the timing of Ozempic’s entry could not be more critical.
What Are Fat Loss Drugs in India
Fat Loss Drugs in India primarily refer to a new class of medicines based on GLP-1 (Glucagon-Like Peptide-1) receptor agonists. These drugs were initially created to help people manage blood sugar levels but later showed strong results in reducing appetite and body weight.
Popular GLP-1 based drugs include
- Ozempic (Semaglutide)
- Wegovy
- Rybelsus (oral version)
- Mounjaro (Tirzepatide – not yet widely available in India)
These medicines are taken either as weekly injections or daily pills, under medical supervision.
A Game-Changer
The launch of Ozempic has pushed Fat Loss Drugs in India into the mainstream conversation. Novo Nordisk introduced Ozempic as a Type-2 diabetes treatment, but global studies and real-world usage revealed its strong impact on fat loss and appetite control.
According to multiple international reports, patients using Ozempic experienced
- Reduced hunger
- Slower digestion
- Lower calorie intake
- Significant weight reduction over months
This has made Ozempic one of the most talked-about drugs worldwide.
How GLP-1 Drugs Work in the Human Body
To understand Fat Loss Drugs in India, it is important to understand how GLP-1 hormones function.
GLP-1 is a natural hormone released by the intestines after eating food. It helps the body by
- Increasing insulin secretion
- Slowing stomach emptying
- Reducing hunger signals to the brain
- Controlling blood sugar levels
GLP-1 based drugs mimic this hormone, making the body feel full faster and for longer durations. As a result, calorie intake reduces naturally, leading to gradual and sustained fat loss.
Fat Loss Drugs in India and the Diabetes Crisis
India is often called the diabetes capital of the world. A 2023 study published in The Lancet Diabetes & Endocrinology revealed that over 101 million people in India are living with diabetes, with the majority suffering from Type-2 diabetes.
Despite awareness campaigns under the National Health Mission (NHM), diabetes remains a major public health challenge.
Fat Loss Drugs in India are now being seen as a dual-purpose solution
- Managing diabetes
- Tackling obesity, which is a major risk factor
Scientific Evidence Behind Ozempic and Weight Loss
Multiple international clinical trials have demonstrated the effectiveness of semaglutide-based drugs.
Key findings include
- Average weight loss of 10–15% over one year
- Improved insulin sensitivity
- Reduced cardiovascular risk
A study published in The New England Journal of Medicine confirmed that patients using semaglutide lost significantly more weight compared to placebo groups.
Benefits of Fat Loss Drugs in India
The growing popularity of Fat Loss Drugs in India is driven by several benefits
Key Advantages
- Clinically proven weight loss
- Better blood sugar control
- Reduced risk of heart disease
- Improved metabolic health
- Appetite regulation without extreme dieting
For patients struggling with obesity and diabetes together, these drugs offer a medical alternative to bariatric surgery.
Risks, Side Effects, and Medical Warnings
Despite the hype, Fat Loss Drugs in India are not risk-free.
Common side effects include
- Nausea
- Vomiting
- Diarrhea
- Constipation
- Fatigue
Serious but rare risks
- Pancreatitis
- Gallbladder issues
- Thyroid tumors (observed in animal studies)
Doctors strongly advise against self-medication. These drugs should only be used under professional medical supervision.
Who Should and Should Not Use These Drugs
Fat Loss Drugs in India are generally prescribed for
- Adults with Type-2 diabetes
- Individuals with BMI above 30
- Patients with obesity-related health conditions
Not recommended for
- Pregnant or breastfeeding women
- People with thyroid cancer history
- Patients with severe gastrointestinal disorders
Medical screening is essential before starting treatment.
Cost, Availability, and Accessibility in India
One of the biggest concerns around Fat Loss Drugs in India is affordability.
Estimated monthly cost
- ₹8,000 to ₹15,000 (varies by dosage)
Currently, these drugs are not covered under most government schemes, making them inaccessible for a large section of the population.
Government Health Programs vs Ground Reality
While the Ministry of Health promotes lifestyle changes under NHM, the growing burden of diabetes and obesity highlights a gap between policy and ground-level implementation.
Experts believe medicines alone cannot solve the problem without
- Nutrition education
- Physical activity promotion
- Early screening programs
Expert Opinions on Fat Loss Drugs in India
Health experts caution against calling these drugs “miracle solutions.”
According to endocrinologists:
“GLP-1 drugs are effective medical tools, not cosmetic weight loss shortcuts.”
Long-term lifestyle changes remain essential for sustainable health outcomes.
Ethical and Social Concerns Around Weight Loss Drugs
The rise of Fat Loss Drugs in India has sparked ethical debates:
- Are these drugs being misused for cosmetic weight loss?
- Will shortages affect diabetic patients?
- Is society promoting medication over healthy habits?
These concerns need urgent regulatory attention.
The Future of Fat Loss Drugs in India
The future looks promising yet cautious. Pharmaceutical companies are investing heavily in next-generation GLP-1 drugs, while Indian regulators are closely monitoring usage patterns.
Experts predict
- Wider availability
- Possible price reductions
- Stricter prescription guidelines
Miracle Cure or Medical Tool
Fat Loss Drugs in India represent a significant medical advancement in tackling diabetes and obesity. However, they are not magic bullets. Used responsibly, under medical guidance, they can improve lives. Misused, they could create new health risks.
As India battles a growing lifestyle disease crisis, the real solution lies in a balanced approach combining medicine, awareness, and healthy living.
We do not provide advice for any medicine; this is only for informational purposes.
Breaking News
hidden sugar in everyday foods is raising your diabetes and heart-disease risk –

Contents
Jaipur, Nov.08,2025:hidden sugar is a term you may have heard casually, but it deserves serious attention. Despite our best efforts to eat healthily, we may unknowingly be consuming large amounts of sugar — not just the lumps of white table sugar, but the sugar that is already embedded in the foods we eat every day. This silent sugar exposure can drive weight gain, type 2 diabetes, heart disease, and other chronic illnesses. With escalating rates of obesity and diabetes globally, it’s time to pull back the curtain and expose the hidden sugar in everyday foods.
In this article we’ll define what hidden sugar really means, show you where it hides, explain how it harms health, review the global trend, and give you actionable tools to detect and reduce it.
What is hidden sugar
By “hidden sugar” we mean sugar that is not obviously present (like a candy bar) but rather appears in everyday foods and drinks that appear healthy, savoury, or innocent. The sugar may be added by manufacturers (so-called “added sugars” or “free sugars”) or may be naturally present but in a form that leads to a rapid blood-sugar spike.
According to the World Health Organization (WHO), “free sugars” include monosaccharides and disaccharides added to foods and beverages by the manufacturer, cook or consumer, and sugars naturally present in honey, syrups, fruit juices and fruit juice concentrates.
Hidden sugar is dangerous because it adds to total sugar intake without you realising it. Many health-organisations warn that the modern diet’s sugar content is far higher than in prior generations, and that much of this comes from processed, packaged or prepared foods. For example, research shows that ultra-processed foods — which tend to contain added sugars, among other additives — are linked to higher risks of type 2 diabetes.
Thus, hidden sugar isn’t just a trivia item — it’s a significant public-health issue.
Everyday foods where hidden sugar lurks
Dairy & yoghurt
Many people assume yoghurt is a health-food. But flavoured yoghurts can contain significant added sugar. The Centres for Disease Control and Prevention (CDC) warns that packaged yoghurts and dairy products may have high amounts of added sugars.
For example, a “fruit-on-the-bottom” cup may have sugar levels comparable to a dessert. Because you expect yoghurt to be healthy, you may not account for that sugar in your daily total.
Bread, buns & bakery items
Bread and bakery items may seem low-risk, but many commercial breads contain sweeteners or sugar to improve texture, aid fermentation, or prolong shelf life. A recent Indian news article flagged that breads and buns often contain more sugar than consumers expect.
Thus something as “innocent” as your sandwich bread may contribute to your hidden sugar load.
Condiments, sauces and “savory” processed foods
One of the biggest culprits for hidden sugar is savoury foods that you wouldn’t suspect: ketchup, pasta sauce, salad dressings, sausages, processed meats. The CDC specifically lists condiments and sauces as common sneaky sources of added sugar.
For example, a single tablespoon of ketchup may already add 3-4 g of sugar.
Drinks, juices and smoothies
Bottled juices, smoothies, energy drinks, flavoured milks — these are classic hidden sugar sources. Even “100 % fruit juice” can contain a high free-sugar load, because fibre is removed during juicing and the sugars act like free sugars.
Also, when you drink sugar rather than eating food, the sugars can be absorbed more rapidly, spiking blood sugar and contributing to metabolic risk.
Ultra-processed snacks and cereals
Breakfast cereals, granola bars, snack foods often carry added sugars under multiple names. Many items marketed as “healthy” may in fact contain sugar as a primary ingredient. The Johns Hopkins Medicine site warns that “whole-grain” or “vitamin-fortified” do not guarantee low sugar.
Artificial intelligence research shows that across many countries, packaged foods often fail to meet carbohydrate-quality benchmarks because of high free-sugar content.
obesity, diabetes, heart disease, and more
When you repeatedly consume hidden sugar beyond what your body can handle, multiple pathways lead to harm.
- Excess sugar contributes to weight gain because it adds calories, often without making you feel full. The WHO says keeping free sugar intake under 10% of total energy reduces risk of overweight and obesity.
- As weight increases, the risk of type 2 diabetes rises. Also, high sugar intake independently can reduce insulin sensitivity.
- Heart disease: hidden sugar plays a role in high blood pressure, inflammation, fatty-liver and cardiovascular risk independent of cholesterol. For example, a recent cardiologist statement claimed sugar may damage the heart more than cholesterol by raising risk up to 21%.
- Ultra-processed food consumption (which usually implies high added sugar) is linked to increased type 2 diabetes risk.
In sum, hidden sugar is not simply “extra sweetness” — it’s an insidious contributor to chronic disease.
rising sugar consumption and the toll on health
Global dietary patterns have changed dramatically in recent decades: processed foods, sugary drinks, high-calorie snacks, and hidden sugar infiltration are widespread. According to recent reporting-
- The WHO guideline suggests reducing free sugars to less than 10% of total energy intake, and ideally below 5% for additional benefits.
- A recent article noted that hidden sugars are “silently increasing health risks like obesity and diabetes” in India, urging awareness of routine foods.
- A machine-learning study found varying compliance across countries in packaged foods meeting carbohydrate-quality standards; some countries had as low as ~9.8% of foods meeting targets.
Thus, hidden sugar is a global phenomenon with local consequences — especially in nations undergoing nutritional transition (such as India, where packaged foods and snacks are growing rapidly).
How to detect and reduce hidden sugar intake
Read labels and watch ingredient lists
One of the first steps is label literacy. The CDC says reading nutrition labels to assess total sugars and added sugars is vital.
Tips-
- Look at “added sugars” or “free sugars” if listed.
- Check the ingredient list: if sugar (or corn syrup, dextrose, fructose, honey, agave nectar) is among the first few ingredients, the product likely has high added sugar.
- Be sceptical of claims like “low-fat” or “whole grain” without checking sugar content.
- Watch serving sizes: what looks small may hide large sugar loads.
Choose whole foods and cook at home
One sure way to avoid hidden sugar- favour unprocessed or minimally processed foods. Fresh vegetables, whole grains, legumes, plain dairy, unflavoured milk/yoghurt. Make your own sauces, dressings, breads. When you control ingredients, you avoid the surprises.
Understand added vs natural sugars
Not all sugars are equal. Sugars naturally present in whole fruits and milk are less problematic because fibre, fat and structure slow absorption. The problem arises when sugars are “free” or added, causing rapid absorption and higher metabolic impact.
Practical switching tips
- Swap flavoured yoghurt for plain yoghurt + fresh fruit.
- Choose breads with minimal added sugar (check label).
- Replace sweetened condiments with homemade versions: e.g., tomato-puree + herbs instead of packaged ketchup.
- Choose water, unsweetened tea/coffee instead of sugary drinks or juices.
- Eat breakfast cereal only if sugar < 5 g/serving or switch to oatmeal with nuts and seeds.
- When buying snacks, pick those with short ingredient lists and no sugar synonyms (corn syrup, maltose, etc.).
body mass index (BMI), health equity & vulnerable groups
While the hidden sugar issue is universal, there are special angles to consider. The common measure of overweight/obesity is the body mass index (BMI), but this measure has limitations: it does not account for body-fat distribution, muscle mass, age, ethnicity. In some ethnic groups (e.g., South Asians) the risk of type 2 diabetes or heart disease may be higher even at lower BMI levels. Thus, relying solely on BMI may mask real risk.
Moreover, hidden sugar harms are affected by social determinants: access to fresh whole foods, education about labels, marketing of processed foods, and socio-economic status. Countries in transition (with rising incomes and shifts to processed-food diets) face steep increases in overweight and diabetes. For example, some forecasts indicate by 2050 over half of adults globally may be overweight or obese if current trends continue.
Therefore the hidden sugar narrative must also include equity: those with fewer resources may be disproportionately impacted.
hidden sugar is more than an inconvenient ingredient — it’s a stealth driver of chronic disease risk. The good news is: awareness and action work. By understanding where sugar hides, reading labels, favouring whole foods, cooking at home, and making smarter swaps, you can significantly reduce your exposure. Given the global rise of obesity, type 2 diabetes and heart disease, uncovering the hidden sugar in your diet is a powerful step toward reclaiming your health.
Breaking News
Back Pain Breast Cancer link revealed — why persistent unexplained back pain may be an early sign and when you must seek medical help-

Contents
Jaipur, Nov.08,2025:Back pain breast cancer might sound alarmist, yet it is a phrase worth remembering. When back pain is persistent, unexplained, grows worse at night or is accompanied by other subtle symptoms—what you think is just “muscle strain” could sometimes signal something far more serious, such as the early stages of breast cancer or its spread. Recent articles highlight that while back pain is rarely due to cancer, in certain instances it may reflect a diagnosis of breast cancer that has progressed or metastasised-
Understanding when back pain is simply benign and when it could be an early warning of breast cancer can empower women to act—and potentially change outcomes.
What the research says on back pain breast cancer
The rarity but significance
Medical research shows that, in the majority of cases, back pain is not caused by cancer. For instance, a review by Dana‑Farber Cancer Institute noted that although 39 % of adults experience back pain each year, the cause is rarely cancer. That said, cases exist where breast cancer that has spread (metastasised) to bones—especially the spine—can cause back pain.
Back pain as a sign of advanced breast cancer
According to a Medical News Today article
“Back pain is more likely to be a symptom of advanced (metastatic or stage 4) breast cancer, which means the cancer has spread to other parts of the body.”
And the UK’s Cancer Research UK confirms bone pain, including back pain, is a common symptom when breast cancer has spread to the bones.
Thus, while back pain breast cancer is not typical in early, localised breast cancer, it can be a red flag of advanced spread.
how it happens
When breast cancer cells spread to the bones of the spine, they weaken bone structure, create pressure or fractures, and irritate nearby nerves — all of which can lead to back pain. Some treatments for breast cancer (like hormonal therapy, chemotherapy) can also cause spine or joint-related pain, adding to confusion.
typical back pain vs back pain breast cancer
Since back pain is extremely common, the challenge is distinguishing benign causes from possible signs of breast cancer. Here are key differentiators-
Typical muscular/back pain features
- Related to movement, posture, lifting, or a sudden strain.
- Improves with rest, stretching, pain-relief measures, or behavioural changes (e.g., better mattress, correct posture).
- Often variable in intensity and location; may improve with time.
Back pain breast cancer features
- Persistent for weeks without clear cause (i.e., not from lifting, posture, pressure) and not improving.
- Occurs or worsens at night, or when lying down.
- May be localised to spine, ribs, pelvis or hips — where breast cancer often spreads.
- Accompanied by other systemic symptoms: unexplained weight loss, fatigue, loss of appetite, swelling, numbness or tingling in limbs.
- Occurs in context of known breast cancer or breast symptoms (lump, discharge, skin change), though sometimes before a breast lesion is detected.
By being aware of these differences, women can be alert to when back pain goes beyond the usual.
Warning signs and red flags of back pain breast cancer
Here are five powerful warning signs every woman should know under the umbrella of back pain breast cancer-
Persistent and Unexplained Back Pain
If your back pain is of unknown origin (no clear injury, no posture cause) and lasts beyond several weeks without improvement, this is a signal. Unlike typical muscle pain, which may ease with rest or therapy, back pain breast cancer-related often continues or worsens.
Night-Time or Resting Pain
Back pain that worsens at night or while lying down—especially when you wake with it or cannot get comfortable—is concerning for possible spinal involvement.
Pain that Spreads or Is Associated with Other Symptoms
If the pain radiates to hips, thighs, ribs or is accompanied by numbness or weakness in limbs—alongside signs like fatigue, weight loss or appetite reduction—it could be more than a strained muscle. The UK Cancer Research site emphasises that bone-spread symptoms often include pain and general signs of decline.
Existing Breast Symptoms + Back Pain
If you already have breast symptoms (lump, discharge, skin change) and back pain arises or persists, you should not ignore it. The link between breast issues and back pain must prompt evaluation.
Known History of Breast Cancer
For women who have had breast cancer before, new or worsening back pain must be evaluated promptly—it may indicate recurrence or metastasis. Even treatments themselves (chemo, hormone therapy) can contribute to back pain, but an evaluation is still warranted.
Why early detection matters for back pain breast cancer
Improved outcomes
When breast cancer—especially one that has begun to spread—is detected early, treatment options widen, and outcomes improve significantly. Although back pain in itself doesn’t guarantee cancer, treating when caught early (for any breast cancer) offers better prognosis.
Avoiding irreversible damage
Bone metastasis, particularly in the spine, can lead to fractures, spinal cord compression, nerve damage, paralysis, or severe pain. For instance, Cancer Research UK says spinal cord compression is an emergency and back pain may be its first symptom.
Distinguishing treatable causes
If back pain is due to benign causes, quick evaluation confirms that and you can return to normal life with peace of mind. If it’s due to breast cancer or spread, early action helps. As a recent article noted:
“Back pain linked to breast cancer: Early warning signs you should never ignore.”
Thus, vigilance over back pain breast cancer isn’t fear-mongering: it is responsible health awareness.
Practical steps if you suspect back pain breast cancer
Here’s what to do if you have back pain and are concerned about its link to breast cancer
Seek medical evaluation
Don’t delay. Tell your doctor that the pain is persistent and unexplained. Provide details: when it started, where exactly, how it feels, what worsens it, whether you have other symptoms, and any breast symptoms/history.
Request appropriate investigations
Depending on your situation, investigations may include:
- Mammogram or breast ultrasound (if you haven’t had one).
- MRI or CT scan of the spine or bones if bone metastasis is suspected.
- Bone scan or PET scan to assess spread to bones or other organs. Medical News Today outlines this process.
Pay attention to self-exams and screening
For all women, regular breast self-exams and screening mammograms (per local guidelines) are critical. If you detect any breast changes (lumps, skin thickening, discharge, nipple inversion) and persistent back pain, act swiftly.
Manage lifestyle and risk factors
While back pain breast cancer may be rare, general breast health helps. Maintain healthy weight, reduce alcohol, stay active, eat a balanced diet, avoid smoking, and maintain a healthy posture and spine-care to reduce benign back pain.
Don’t ignore other signs
Besides back pain, unusual fatigue, unexplained weight loss, bone pain elsewhere, or neurological signs (numbness, weakness) necessitate urgent medical review.
- Back pain breast cancer is rare, but it is a possible sign when back pain is persistent, unexplained and accompanied by other symptoms.
- The probability of back pain being related to breast cancer increases when there are breast symptoms/history or when the pain occurs at night, worsens, or is located in spine/bone zones.
- Early detection of any breast cancer—even when presenting atypically through back pain—improves outcomes and reduces risk of severe complications.
- Regular screening and attunement to your body’s signals are vital. If something feels “off” with your back and you don’t have a clear explanation, don’t dismiss it as mere fatigue or posture-error.
- Always consult a healthcare professional rather than diagnosing yourself.
Back pain breast cancer may not be the most common phrase you’ll hear, but it’s one worth remembering. If you are a woman experiencing back pain that doesn’t resolve, especially alongside any breast symptoms or risk factors, being proactive could make all the difference. Don’t wait—listen to your body, trust your instincts, and seek help when something doesn’t feel right. Early action is powerful.
Breaking News
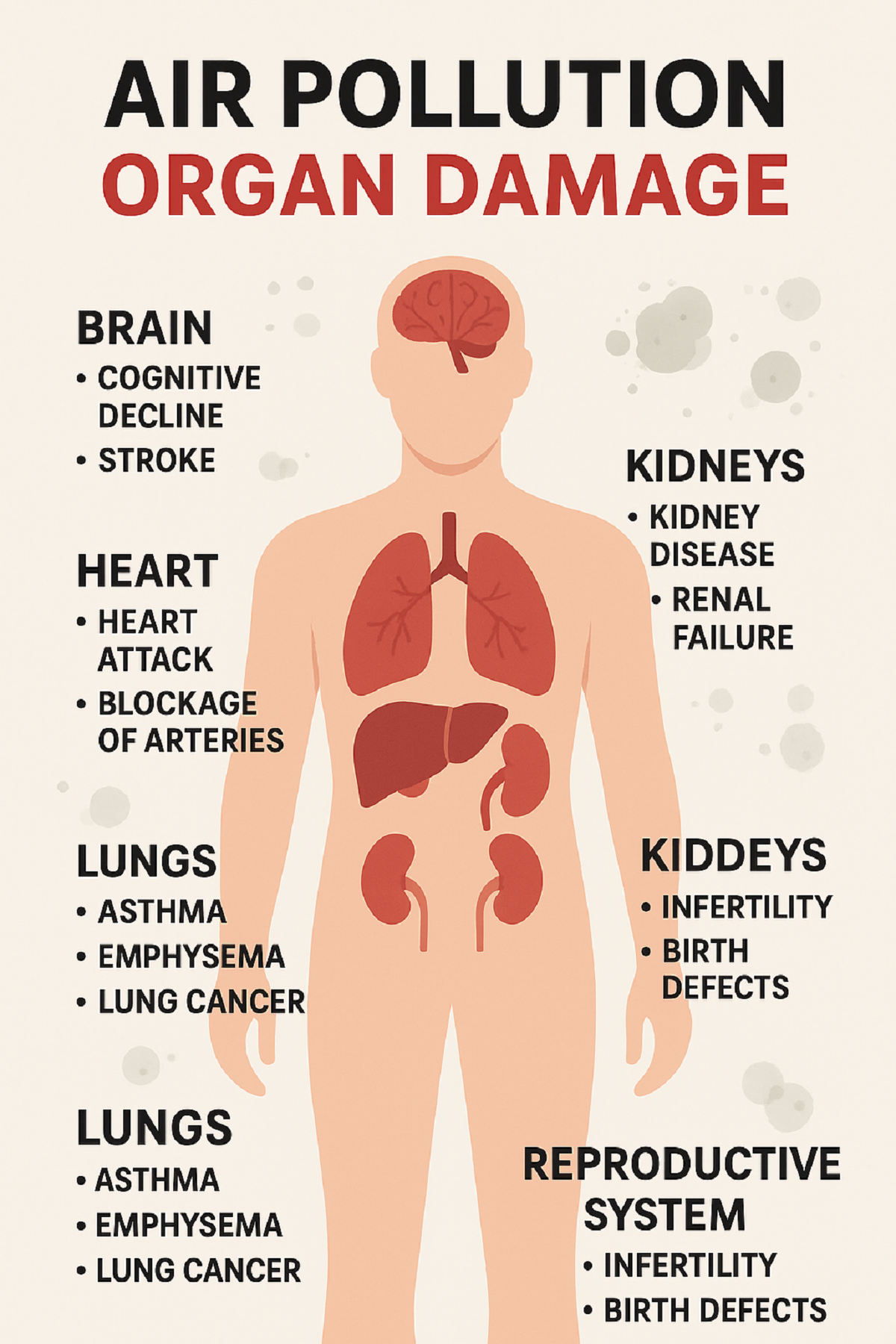
Air Pollution Organ Damage is more than just lung disease—
Contents
New Delhi, Nov.06,2025:When we talk of air pollution, the first thought is often smog, wheezing, or lung problems. But the term Air Pollution Organ Damage captures a wider reality: fine and ultra-fine particles (like PM2.5, PM10, even <0.1 microns), gases (NO₂, CO, SO₂) and toxic chemical compounds infiltrate the body, travel via the bloodstream, and damage multiple organs. Experts now warn that what we breathe in the winter months of Delhi isn’t just making us cough—it’s harming our heart, brain, kidneys and even our reproductive health-
The stakes are huge. According to one article, nearly 15 % of all deaths in Delhi in 2023 were linked to air pollution. That underlines how Air Pollution Organ Damage shifts the conversation from a seasonal nuisance to a full-scale public health emergency.
The science behind how polluted air harms organs
Particulates, nano-particles & bloodstream entry
Particles with aerodynamic diameter less than 2.5 microns (PM2.5) can reach deep into the alveoli of the lungs; even ultrafine particles (<0.1 microns) can penetrate the alveolar–capillary barrier, enter the bloodstream and move to organs. As one doctor described: “Fine particles … not only reach the lungs they can cross into the bloodstream and travel to all parts of the body.”
Systemic inflammation & oxidative stress
Once in circulation, these particles trigger chronic inflammation and oxidative stress. The body’s immune response remains persistently activated, causing damage to blood vessels, tissues and organs over time. According to research from India: “air pollution is worsening anaemia, hypertension, diabetes, cholesterol levels and mental health” alongside more traditional lung impacts.
Mechanisms of organ damage
- Cardiovascular system: Pollutants cause narrowing of arteries, increased blood pressure, plaque formation, heart rhythm abnormalities and risk of heart attack.
- Brain and nervous system: Particles can trigger neuroinflammation, increase risk of stroke, dementia, cognitive decline and mood disorders.
- Reproductive system: Studies indicate that exposure to air pollution reduces sperm quality, increases infertility, and affects fetal growth and development.
- Kidneys and liver: Pollutants have been associated with kidney disease, liver damage, and metabolic disorders like diabetes.
In effect, Air Pollution Organ Damage is not an “additional risk”- it is already woven into the fabric of life for many in high-pollution zones.
heart, brain, kidneys, reproductive system & more
Heart and cardiovascular system
The risk increase is evident. A study shows that “even a slight spike in PM2.5 can increase risk of heart attack by 2.5 per cent the very same day”. Another analysis emphasised that particulate matter leads to plaque formation, narrowed arteries and elevated blood pressure, all contributing to heart attacks and strokes. These reflect core components of Air Pollution Organ Damage.
Brain and cognitive health
Air pollution’s effects on the brain are only recently being appreciated. As one expert noted: “It’s harming your brain, too … how toxic air affects your heart, brain, and children’s growth.” The implications: increased risk of dementia, reduced cognitive ability in children, mood disorders, memory issues. Those are major pieces of the Air Pollution Organ Damage puzzle.
Kidneys, liver and metabolic health
Studies based in India reveal strong associations between polluted air and hypertension, diabetes, anaemia and lipid disorders. Once again, Air Pollution Organ Damage extends beyond visible symptoms to metabolic and organ-level dysfunction.
Reproductive system and children’s health
Children and pregnant women face a double jeopardy. Exposure can lead to reduced lung growth, developmental delays, lower IQ, pre-term birth, intra-uterine growth retardation and congenital abnormalities. For adults too—infertility, reduced sperm count and reproductive disorders are increasingly linked to poor air quality—part of the broader sweep of Air Pollution Organ Damage.
Other organs and systems
Beyond the major ones above: chronic exposure affects immune system regulation, skin barrier function, and even eyes (allied organs). One article states- “Even animals… pollutant entry can reach skin, brain, kidneys, liver and more.”
Who is most vulnerable to Air Pollution Organ Damage
Children and teenagers
Because lungs, brains and bodies are still developing, children absorb more pollutants relative to body size, breathe faster, and thus suffer greater long-term consequences.
Elderly and those with pre-existing conditions
Those with heart disease, lung ailments (COPD/asthma), diabetes or weakened immunity are at higher risk of organ damage from pollution.
Pregnant women and unborn children
The “fetal programming” effect means prenatal exposure leads to future health burdens: childhood disorders, developmental delays, chronic conditions.
General population in high-pollution zones
Crucially: even “healthy” adults are not immune. Short-term exposure can trigger cardiovascular or neurological effects.
In short, when we consider Air Pollution Organ Damage, the vulnerable populations are broad, and the risk extends to virtually everyone exposed to long-term or high-level pollution.
Real-life data from Delhi-NCR making the crisis visible
AQI and smog levels
In Delhi and NCR, the onset of winter invariably brings a surge in AQI values into the “poor” to “severe” range. Local data show weekly AQI sometimes hitting 350–400 in certain localities. (“Every year… AQI worsens with winter.”)
Mortality linked to air pollution
Recent analysis: In 2023, nearly 15 % of all deaths in Delhi were linked to ambient air pollution.
Evidence of organ damage beyond lungs
- A Times of India article reported: “Exposure to even one hour of toxic smog can… trigger kidney, liver, fertility problems.”
- An Indian Express piece: “A slight spike in PM2.5 can increase risk of heart attack by 2.5 % the same day.”
- NDTV article: “Ultrafine particles can enter the bloodstream, reaching organs such as the heart, brain and kidneys.”
Together these show how Air Pollution Organ Damage is already operating in the field—not just as theory but as data-driven reality.
How to protect yourself from Air Pollution
Since Air Pollution Organ Damage spans across organs, the protective strategy must be multi-layered.
Indoor protection
- Use air purifiers, especially in bedrooms and living rooms, although they don’t offer complete protection.
- During severe pollution days, minimize opening windows; keep recirculate mode turned on in ACs.
Outdoors and behavioural changes
- Wear N95/N99 masks correctly when stepping out during high AQI days. Experts emphasise correct fit.
- Avoid exercise/outdoor activities early morning or late evening during smog peaks.
Health-oriented lifestyle
- A diet rich in antioxidants helps combat oxidative stress triggered by pollutants.
- Stay hydrated, sleep well, avoid smoking or other pollutants.
- For pregnant women or families with children: monitor air quality, avoid exposure peaks, follow paediatric/adult physician guidance.
Community & systemic awareness
- Keep track of local AQI dashboards. In Delhi: visit or similar sites.
- Be aware of susceptible times: crop-burning season (post-monsoon/winter), temperature inversions, low wind.
While personal measures are important, they are only part of the solution—because the root cause is ambient.
The policy and systemic gap
Inadequate recognition of organ-wide damage
Despite mounting evidence, policies still emphasise respiratory illness. The term Air Pollution Organ Damage is rarely used in official discourse. Studies show that while respiratory and cardiovascular links are known, metabolic, renal and neurological effects are less addressed.
Enforcement and real-time action lag
High-pollution episodes follow stubble-burning, vehicular emissions, industrial output and urban dust. While there are curbs (podies, fire-cracker bans), systemic enforcement in high-pollution zones remains weak.
Healthcare system readiness
Many physicians are trained to treat lung or heart issues, but aren’t routinely linking them to ambient air pollution as underlying cause. Research shows health and environment departments operate in silos.
Public awareness & shifting narrative
Popular perception still limits pollution damage to lungs. Framing it as Air Pollution Organ Damage—spanning brain, heart, fertility, kidneys—could mobilise stronger public and political action.
The cost of inaction
Reduced life expectancy, increased burden of chronic disease, greater healthcare costs and productivity loss all flow from unchecked Air Pollution Organ Damage. Recognising and acting on it is not optional—it’s imperative.
Air Pollution Organ Damage is not a remote future scenario—it is playing out now among millions, particularly in regions like Delhi-NCR. What began as visible lung-disease has widened into a systemic assault on our bodies. From hearts and brains to kidneys and reproductive systems, the evidence is clear: the air we breathe matters.
Andhra Pradesh
pregnant-weightlifting-145kg-feat-redefines-strength-

Contents
Andhra Pradesh, Oct.31,2025:Pregnant weightlifting has entered the public consciousness in a dramatic way, as one woman’s extraordinary feat pushes the boundaries of strength, motherhood and societal expectation. The story of this lift—145 kg at seven months’ pregnancy—sparks both awe and debate- what happens when pregnancy meets serious athletic performance-
Who is the athlete behind the lift
The central figure is Sonika Yadav, a constable in the Delhi Police, who competed in the All India Police Weightlifting Cluster 2025‑26 held in Andhra Pradesh.
Her back-story adds layers to this achievement-
- She joined the Delhi Police in 2014 and has been active in sports, including kabaddi and powerlifting.
- In 2022 she began a more rigorous fitness journey when she was considerably overweight and struggling with lifestyle diseases. She shifted into weightlifting training.
- In 2023 she won gold in a state deadlift competition and then, when she realised she was pregnant, instead of stepping back she chose to continue with medical supervision.
Her motivation: to break the narrative that pregnancy equals pause; she has said she wanted to show that motherhood and athletic ambition can go hand-in-hand.
145 kg and a bronze medal
During the competition, Sonika lifted a total of 145 kg in the deadlift portion, while being seven months pregnant.
Specifically-
- She first performed 125 kg in squats, 80 kg in bench-press, then moved on to a planned 135 kg deadlift but raised it to 145 kg.
- She secured a bronze medal in the 84 kg category at the All India Police Weightlifting Cluster.
- In her own words: she didn’t want pregnancy to be seen as a limitation, and she thought: “If they [other pregnant athletes] can do this, why can’t I?”
This event has been widely shared on social media and covered by major news outlets, capturing public attention for both its positive and contentious implications.
Public reaction
The achievement generated a two-fold reaction: celebration and concern.
The celebration
Many applauded the boldness and determination of Sonika — a woman in uniform, yet also a mother and soon-to-be mother, showing strength in every sense. Her message: pregnancy isn’t a weakness. Her story inspired many who feel sidelined by cultural expectations.
The alarm
On the flip side, commentators raised questions about safety. Some described the act as “risky” or “irresponsible”, warning that heavy lifting while pregnant could endanger the mother and unborn child. According to one report:
“…questions whether heavy occupational lifting during pregnancy is safe.”
This mix of praise and caution places pregnant weightlifting in a contested zone — between empowerment and risk.
Is pregnant weightlifting safe
What experts say
According to senior obstetrician Dr. Nikhil Datar, each pregnancy is unique-
“Some women with medical clearance and supervision can continue strength-training safely. But this case is special – an athlete with years of training.”
He cautions:
“Heavy occupational lifting or high-intensity sets are not generally recommended.”
Key considerations
When assessing pregnant weightlifting the following matter-
- The woman’s baseline fitness level and training history (in this case, years of powerlifting).
- Medical clearance and ongoing monitoring. Sonika reported she consulted her doctor and continued under supervision.
- The intensity and load: what constitutes “heavy” weight differs based on individual capacity.
- The stage of pregnancy: Seven months is advanced, and physiological changes (hormones, joint laxity, heart rate, oxygen demands) become significant.
- The difference between recreational strength training and competitive heavy lifts in a setting.
Thus: pregnant weightlifting can be done safely under certain conditions — but what Sonika did is exceptional, not standard.
Guidelines for strength training during pregnancy
Given the above, what can pregnant individuals consider if they want to stay active through strength training? Below are general guidelines (not personalised advice)-
Consult your healthcare provider
Always begin with a prenatal check-up and get a plan tailored to your health, fitness history, and pregnancy stage.
Choose appropriate load and intensity
- Focus on moderate resistance: safe strength work rather than maximal lifts.
- Avoid sudden heavy loads or maximal single-reps unless under expert supervision.
- For example: walking, body-weight strength, supervised machines may be preferable.
Monitor your body’s signals
Be attentive to-
- Pelvic, abdominal or back pain.
- Dizziness or breathlessness.
- Swelling or reduced foetal movements.
- Joint instability (due to pregnancy hormones).
Prioritise position, posture and stability
- Use machines or supported benches rather than unstable loads.
- Avoid lying flat on back after first trimester if instructed by physician.
- Maintain core engagement, minimise valsalva (holding breath during lift).
Avoid extremes
High-intensity or heavy occupational lifting (e.g., very heavy deadlifts) carry higher risk and require expert monitoring. As Dr. Datar notes, Sonika’s case is not the baseline.
Shift goals from “performance” to “health and wellness”
During pregnancy, the goal can shift: maintain strength, promote circulation, assist recovery and mood — rather than chasing personal records.
For further reading on exercise in pregnancy see the NHS guidance or the American College of Obstetricians and Gynaecologists (ACOG) resources.
The bigger narrative
Beyond the technicalities, Sonika’s story speaks to bigger themes surrounding pregnant weightlifting and women’s roles in society.
Challenging the “pause” narrative
In many societies, pregnancy is framed as a period of rest, withdrawal or at least drastically reduced activity. Sonika turned that on its head-
“I didn’t want pregnancy to be seen as a limitation.”
Role-modelling strength for women
Her lift sends a message: a woman can be a mother, a professional (police officer) and an athlete — roles often siloed by expectation. The wider public reaction (both cheers and criticisms) spotlights how unusual this is still considered.
A conversation starter on risk, agency and support
While not everyone should attempt what she did, her choice raises the question: how much agency do pregnant women have in shaping their bodies, ambitions and physical lives? And how many feel constrained by societal expectations of motherhood?
What her story signals for the future of sport
Sporting bodies have begun adapting for pregnant athletes (e.g., in track and field, team sports). The question of pregnant weightlifting invites reflection on how training protocols, coaching, athlete-care and cultural practices might evolve.
What this means for women in sport
Pregnant weightlifting may sound provocative, even controversial—but the story of Sonika Yadav shows that with preparation, guidance, and experience, boundaries can be pushed.
What we learn-
- Fitness and ambition need not stop during pregnancy — but must be recalibrated.
- Every pregnancy differs; what’s feasible for one woman isn’t for another.
- Societal narratives around pregnancy often restrict rather than empower; stories like this challenge them.
- Fitness professionals, doctors and athletes must collaborate more deeply to develop safe pathways for pregnant athletes.
Caution remains important. This is not a call for every pregnant woman to take up heavy deadlifts. Instead, it signals an evolving understanding of what pregnancy can look like in terms of physicality and agency.
Breaking News
Mental health crisis in India youth with new data- from soaring anxiety & depression to the hidden pressure of social media-
Contents
New Delhi, Oct.14,2025:Mental health crisis in India youth is no longer a whisper from the fringes—it has become a loud alarm that demands attention. Across urban and rural regions, among students and young professionals, anxiety, depression, emotional distress, and suicidal thoughts are rising sharply. This article unpacks the data, digs into the causes, and highlights what can be done before the crisis deepens further-
Alarming statistics- how widespread is the issue
Study in Tier-1 cities
A recent study conducted by SRM University AP, Amaravati, published in the Asian Journal of Psychiatry, surveyed 1,628 students (aged 18–29) across eight major Indian cities (Delhi, Mumbai, Bengaluru, Chennai, Hyderabad, Pune, Ahmedabad, Kolkata). Findings include:
- Nearly 70% of students reported moderate to high anxiety.
- About 60% showed signs of depression.
- Over 70% felt emotionally distressed.
- 65% struggled to regulate behaviour or emotions.
Other relevant data
- Among adolescents in Telangana and Karnataka (ages 10-18), over 60% reported sleep difficulties; 70% reported problems focusing in class.
- In India’s workforce and academic settings, nearly 75% of high school students sleep fewer than 7 hours due to late-night social media use; many feel career uncertainty.
- UNICEF reports indicate only 41% of young people in India believe it’s good to seek help for mental health problems, compared to ~83% in many other countries.
- Treatment gap and professional shortage
- India has about 0.75 psychiatrists per 100,000 people, far below WHO recommendations.
- Treatment gap for mental disorders is estimated between 70% to 92%, depending on region and disorder.
These numbers show that mental health crisis in India youth is wide, serious, and multi-dimensional.
Case studies- when social media becomes a trigger
While data gives scale, real stories show the human toll. They mirror many of the trends uncovered by recent studies and add urgency to the need for prevention.
- Case 1: In Raipur (Chhattisgarh), a 22-year-old man who made reels and videos felt despair when his recent posts didn’t get many views. He increasingly isolated himself and one day injured himself via cutting his wrist. Family intervened just in time and got medical help.
- Case 2: In Bhopal, a 23-year-old woman preparing for competitive exams felt immense pressure, loneliness, and repeated failures. She attempted suicide when she felt she had no outlet—this, despite being academically good. Intervention came in time, with help from family and mental health professionals.
These stories underline how external validation (likes, views, status), social isolation, peer comparison, and academic pressure can interact with vulnerabilities, causing crises.
pressure, lifestyle, pandemic impact
Academic, peer & social media pressure
Students cite overwhelming competition, expected academic success, job prospects, etc. Social media amplifies peer pressure: lifestyle comparisons, social status, likes/views become measures of self-worth. Studies show high social media usage correlates with anxiety, sleep issues, and emotional distress.
Lifestyle changes and lack of physical activity
In many cases, children and young adults have decreased physical activity, increased screen time, poor sleep habits, and irregular routines. These contribute to emotional instability, mood disorders, and even physical health issues. This is in line with child psychiatry experts’ observations. (Your original cases about media, gaming addiction, lack of physical activity illustrate this.)
Pandemic after-effects and isolation
COVID-19 lockdowns, disruptions in schooling / college, increased remote/online interactions have caused prolonged isolation. Reports show that youth aged 18-24 were among the worst affected in their mental health scores post-pandemic.
Lack of early support, stigma & awareness
Although awareness has increased, many young people do not recognize early signs. Many are reluctant to seek help due to fear of being judged or due to lack of access. UNICEF data shows low rates of belief in seeking mental health support in India relative to other countries.
physical and psychological links
The mental health crisis in India youth doesn’t only affect emotions—it has broader health and social consequences.
- Physical health risks: Conditions like hypertension, diabetes, heart disease are rising in tandem with mental stress. Stress hormones affect sleep, diet, and bodily systems. In your source data, psychiatric experts note links between mental distress and these physical disorders.
- Emotional regulation & behaviour problems: Youth may have difficulty managing mood, behaviour, impulsivity. Increased substance use, self-harm, or suicidal ideation may follow, especially when pressure or rejection (e.g. from social media) is perceived.
- Academic, social, relational impact: Decline in performance, drop in self-esteem, withdrawal from friends/family, breakdowns in relationships. As in the cases you describe.
- Long-term risk: Early mental health conditions often predict recurrent problems, even in later adulthood. Unaddressed depression or anxiety may lead to chronic illness, lower life satisfaction.
studies, support systems, campaigners
University & survey reports
- The SRM University AP study (1,628 students) as mentioned above.
- Studies on adolescent girls’ mental health, including awareness programmes in remote or rural areas (e.g. Assam, Telangana).
Helplines & tele-mental health
- Tele-MANAS in Karnataka has received over 65,000 calls since its launch in 2022, supporting young people in crises.
- New mental health helpdesk for medical students in Telangana (T-JUDA) to offer peer support, counselling.
Government & policy efforts
- Economic Survey 2024-25 underscores need for preventive mental health education, digital services, workplace policies.
- UNICEF’s “Mental Well-being for Young People” approach that emphasizes integrated services, early detection, reducing stigma.
Community, grassroots action
- Peer-led programmes, student support groups, awareness in schools.
- Workshops and community health clinics in tribal or rural areas improving access (e.g. Gadchiroli study).
What needs to change-solutions and early interventions
To address the mental health crisis in India youth, multiple coordinated steps are essential:
Early identification & screening
- Integrate mental health screening in schools, colleges. Trained counsellors should observe signs: sleep problems, withdrawn behaviour, changes in mood or performance.
- Use validated tools, possibly AI/technology-assisted where feasible, especially after the rise in digital mental health studies.
Awareness & destigmatization
- Reduce shame attached to mental illness. Public campaigns, peer testimonials, role models speaking out.
- Educate parents, teachers, employers about what mental illness may look like, that it can be treated, and help exists.
Improve access to professional care
- Increase number of psychiatrists, psychologists, psychiatric social workers. WHO recommendation is higher than current ratio.
- Enhance tele-mental health services: helplines like Tele-MANAS, online counselling.
Support systems in institutions
- Schools and colleges should have counselling centres, peer support cells. Emotional support should be part of curriculum.
- Employers should build policies allowing mental health days, wellbeing programs, reduce burnout.
Healthy lifestyle & digital balance
- Promote physical activity, sleep hygiene, limits on screen time.
- Teach young people digital literacy: how social media works, how comparison and algorithms can amplify distress.
turning awareness into action
The mental health crisis in India youth is a reality. It’s visible in statistics, in heartbreaking case studies, and in every city and rural area where young people suffer in silence. But there is also hope. Awareness is rising. Institutions, researchers, policy makers, and community actors are stepping in.
Breaking News
Excess Rice and Roti Consumption Linked to Rising Diabetes Risk in India – ICMR Study 2025-

Contents
New Delhi, Oct.10,2025:The ICMR Study 2025 has issued a stark warning to Indian households: overconsumption of rice and roti — staples of the Indian diet — could be driving an alarming rise in diabetes, obesity, and metabolic disorders across the country. Conducted by the Indian Council of Medical Research (ICMR) in collaboration with the Madras Diabetes Research Foundation (MDRF), this large-scale study offers deep insight into how India’s eating patterns are affecting public health-
According to the research, 62% of India’s daily energy intake comes from carbohydrates, primarily white rice, wheat, and processed grains. These foods, though culturally integral, are significantly contributing to poor metabolic health outcomes.
High Carbohydrate Dependence in Indian Diets
The ICMR Study 2025 examined food consumption habits across 30 states and union territories, involving adults aged 20 years and above. The results reveal a concerning pattern — most Indians rely heavily on refined carbohydrates while consuming inadequate protein and fibre.
The data showed-
- Carbohydrates: 62.3% of total daily energy
- Fats: 25.2%
- Proteins: only 12%
The study also highlighted that processed grains contribute 28.5% and whole grains contribute 16.2% to total carbohydrate intake. Such an imbalance between nutrient groups makes Indians highly vulnerable to metabolic conditions like Type 2 diabetes and obesity.
Diabetes and Obesity Connection Explained
Published in Nature Medicine, the ICMR study notes that individuals consuming the highest levels of carbohydrates are 30% more likely to develop diabetes compared to those on low-carb diets. Additionally, the risks of general obesity increase by 22% and abdominal fat accumulation by 15%.
India already accounts for nearly one-fourth of the world’s diabetes cases, a number that continues to grow faster than in most countries. The report attributes this to excessive carbohydrate consumption, coupled with a sedentary lifestyle.
Processed vs Whole Grains – The Hidden Truth
While traditional wisdom suggests that whole grains like millets or brown rice are healthier alternatives, the ICMR Study 2025 warns that merely switching from processed to whole grains may not be enough.
The research indicates that even unprocessed wheat or millet flours do not significantly reduce diabetes risk when consumed in excess. This is because high carbohydrate intake — regardless of its source — leads to elevated blood sugar and insulin resistance over time.
Nutrition experts emphasize balancing grains with protein-rich foods and fibre, which help slow down sugar absorption.
What Experts Are Saying About the Findings
Dr. Vibhuti Rastogi, Senior Dietitian at the Institute of Human Behaviour and Allied Sciences (IHBAS), told that Indian diets are indeed “too carb-heavy and too low in protein,” which accelerates the onset of lifestyle diseases.
“Both refined and simple carbohydrates, such as sugar, can increase diabetes risk. But when combined with low protein intake, the damage happens faster,” Dr. Rastogi explained.
Similarly, Nazneen Hussain, Head Dietitian at Dietetics for Nutrify Today (Mumbai), highlighted that the type of carbohydrate also matters.
“If you eat rotis made from refined flour, they’re almost as bad as polished rice. Choose coarse or fibre-rich flour to slow blood sugar spikes,” she advised.
She also noted that brown rice or unpolished small-grain rice are healthier alternatives but must be eaten in moderation and with fibre, dal, or vegetables for balance.
Regional Differences in Health Risks
The study found striking regional variations in obesity and metabolic disease rates:
- North India: 54% overweight, 37% obese, and 48% had abdominal obesity
- East India: Showed the best metabolic health indicators nationwide
- Overall: 83% of participants showed at least one metabolic risk factor
Additionally, 27% of adults nationwide suffer from hypertension, a condition often linked with excess carbohydrate and sodium intake. Interestingly, these trends showed little regional difference — indicating a nationwide dietary imbalance.
How to Reduce Carbohydrate-Related Health Risks
Experts recommend gradual dietary transitions rather than drastic eliminations. Here’s how to make daily Indian meals healthier, based on ICMR’s recommendations:
- Reduce refined grains: Replace white rice with brown rice, millets, or quinoa.
- Increase protein intake: Add dals, paneer, eggs, tofu, or lean meats.
- Add healthy fats: Use nuts, seeds, and olive or mustard oil instead of saturated fats.
- Control portion sizes: Especially for rice and roti at dinner.
- Include fibre-rich foods: Vegetables, salads, and legumes improve digestion and metabolism.
Lifestyle Changes to Control Diabetes Risk
Beyond diet, the ICMR Study 2025 found that 61% of participants were physically inactive. Regular exercise can reduce Type 2 diabetes risk by up to 50%, according to global health data.
Recommended lifestyle changes–
- Walk or exercise at least 30 minutes daily
- Practice yoga or light resistance training
- Limit sugary drinks and late-night snacking
- Sleep 7–8 hours daily
- Get routine blood sugar check-ups, especially if above 30
Combining these habits with balanced nutrition can reverse early-stage metabolic disorders, experts say.
The Way Forward for a Healthier India
The ICMR Study 2025 is a wake-up call for India’s food culture. While rice and roti remain dietary staples, overreliance on these high-carb foods is quietly eroding public health. With nearly 83% of adults showing metabolic risks, the nation must rethink its traditional plate.
Nutrition experts unanimously agree — moderation, balance, and movement are key. By incorporating more proteins, healthy fats, and fibre, alongside regular physical activity, India can curb the rising tide of diabetes and obesity.

















