Health
Understanding the Genetic Connections: DNA Traits and the Risk of Smoking-Related Cancers
Contents
Introduction to Smoking-Related Cancers
Smoking-related cancers represent a significant public health challenge, with tobacco use being one of the leading causes of preventable diseases. Epidemiological studies have shown a strong correlation between smoking and various types of cancer, notably lung cancer, which accounts for a substantial proportion of cancer deaths worldwide. In fact, approximately 85% of lung cancer cases are attributable to smoking, a statistic that underscores the serious health risks associated with tobacco use. Beyond lung cancer, smoking is also linked to cancers of the mouth, throat, esophagus, pancreas, bladder, stomach, and cervix, among others.
The prevalence of smoking-related cancers is alarming; according to the World Health Organization, tobacco kills more than 8 million people each year, a significant number of whom develop cancer as a direct consequence of their smoking habits. What makes this health crisis even more complex is the fact that individuals exhibit varying risk factors for developing smoking-related cancers. Genetic predispositions, lifestyle choices, and environmental exposures can all influence an individual’s susceptibility to these malignancies, suggesting that risk is not uniformly distributed across the population.
Understanding the factors that contribute to smoking-related cancers is crucial not only for prevention efforts but also for developing effective treatment strategies. For instance, research into genetic connections can provide insight into why some smokers may develop cancer while others do not. By recognizing the multifaceted nature of these risk factors, healthcare providers can target interventions more effectively, tailoring strategies to meet the specific needs of individuals based on their unique risk profiles. This nuanced understanding emphasizes the importance of both genetic and environmental influences in the fight against smoking-related cancers.
The Role of DNA in Cancer Risk
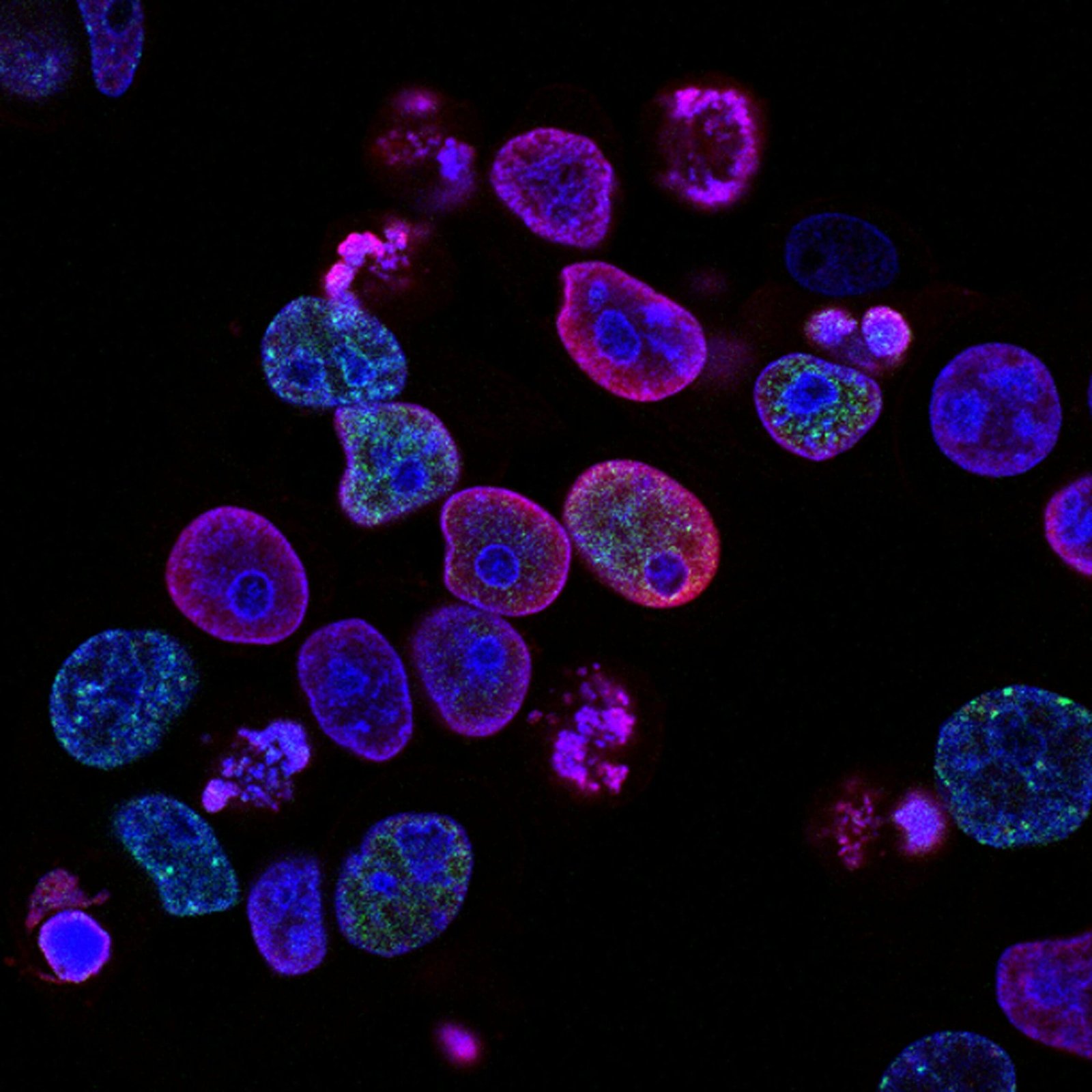
Cancer susceptibility is a complex intersection of environmental factors and genetic predispositions, with DNA playing a pivotal role in determining an individual’s risk. The genetic makeup of a person, encapsulated within their DNA, contains specific traits that may predispose them to various types of cancer, particularly those associated with smoking. Smokers are more likely to develop specific malignancies such as lung cancer; however, not all smokers are equally susceptible, suggesting the influence of genetic factors.
Scientific research has identified various DNA mutations and polymorphisms that can affect an individual’s ability to metabolize carcinogens present in tobacco smoke. For instance, genes involved in detoxification processes, such as CYP1A1, have been shown to influence how efficiently certain carcinogens are processed within the body. Individuals with specific mutations may accumulate higher levels of these harmful substances, thus increasing their risk for developing cancer.
Furthermore, DNA traits associated with DNA repair mechanisms also play a crucial role. Genes such as BRCA1 and BRCA2, known for their involvement in the repair of damaged DNA, can impact an individual’s susceptibility to cancers. A compromised ability to repair DNA can lead to the accumulation of mutations, further enhancing cancer risk, particularly with continued exposure to smoking. The interplay between these genetic traits and environmental exposure illustrates the importance of personalized medicine, where genetic screening could help identify individuals at heightened risk for smoking-related cancers.
As our understanding of the genetic underpinnings of cancer risk deepens, it becomes increasingly apparent that DNA traits are significant contributors to individual vulnerability. By investigating these genetic factors, researchers aim to tailor prevention and treatment strategies that consider not only lifestyle choices like smoking but also an individual’s unique genetic profile.
Research Overview: Linking DNA to Cancer and Smoking
Recent studies have increasingly focused on exploring the intricate relationship between genetic factors, smoking behavior, and the risk of developing smoking-related cancers. This growing body of research aims to identify specific DNA traits that may predispose individuals to these cancers, thereby elucidating how genetics and lifestyle choices interweave to influence health outcomes. One prominent approach in this field is the utilization of genome-wide association studies (GWAS), which analyze thousands of genetic variants across genomes to pinpoint those that correlate with cancer risk.
One notable finding from recent GWAS indicates that certain single nucleotide polymorphisms (SNPs) are significantly associated with an increased risk of lung cancer among smokers. These SNPs underscore the genetic vulnerability of individuals who smoke, suggesting that while smoking is a modifiable risk factor, underlying genetic predispositions can amplify its cancerous effects. Additionally, epigenetic studies have revealed how smoking can alter gene expression, creating a complex feedback loop where genes influence smoking behavior and vice versa.
Another vital methodology leveraged in this research is the use of biomarker identification, which explores how particular genetic markers can signify an individual’s susceptibility to cancer based on their smoking history. For instance, certain variants have been linked to a higher likelihood of developing bladder and throat cancer in smokers. These findings are crucial as they extend beyond merely associating smoking with cancer; they also provide insights into preventative strategies tailored to individuals based on their genetic profiles.
The implications of these studies are profound. Understanding the genetic connections to smoking-related cancers emphasizes the importance of personalized medicine. As researchers continue to delve deeper into the genetic landscape, their findings could inform screening processes, risk assessments, and ultimately, cancer prevention strategies tailored to genetic predispositions. Therefore, this research not only contributes to the theoretical framework surrounding cancer and smoking but also enhances practical applications in public health and clinical settings.
Identifying Genetic Markers for Smoking-Related Cancers
Recent advances in genetic research have significantly expanded our understanding of how certain genetic markers may contribute to the risk of developing cancers associated with smoking. These markers serve as identifiable indicators within an individual’s DNA that can help predict susceptibility to such cancers. A variety of studies have pinpointed specific genes that, when altered, may heighten the risk of conditions like lung and throat cancer, specifically in individuals with a history of tobacco use.
One prominent example is the variations in genes involved in the metabolism of carcinogens found in tobacco smoke. Genetic polymorphisms in the CYP1A1 and GSTM1 genes have been associated with increased carcinogenicity in smokers. The CYP1A1 gene plays a crucial role in the metabolism of polycyclic aromatic hydrocarbons, which are a significant component of tobacco smoke. Alterations in this gene can lead to an increased susceptibility to lung cancer. Additionally, the GSTM1 gene is responsible for encoding proteins that help detoxify harmful substances; the null variant of GSTM1 has been linked with a higher risk profile in smokers.
Identifying these and other specific genetic markers is essential not only for understanding the biological mechanisms underlying smoking-related cancers but also for guiding future research and potential screening methodologies. Researchers are increasingly focusing on whole-genome sequencing approaches to uncover even more genetic variants associated with cancer risk in smokers. The identification of these markers can facilitate personalized medicine, allowing healthcare professionals to tailor screening strategies and preventive measures based on an individual’s unique genetic makeup, ultimately leading to more effective cancer risk management.
The Interaction of Genetics and Environment in Cancer Risk
The interplay between genetics and environmental factors is a critical aspect in understanding the risk of smoking-related cancers. Individual genetic predispositions can significantly influence how environmental elements, such as tobacco exposure, affect cancer development. Genetic variations, especially in genes responsible for metabolizing carcinogens found in tobacco smoke, can alter an individual’s susceptibility to the harmful effects of smoking. For instance, certain polymorphisms in the CYP1A1 gene have been associated with an increased risk of lung cancer among smokers, indicating that genetic makeup plays a vital role in modulating cancer risk.
Furthermore, it is important to consider that not all smokers possess the same level of risk for smoking-related cancers. The presence of specific inherited traits can steeply increase the chance of developing these malignancies when combined with environmental exposures. This is known as a gene-environment interaction. Smokers who carry particular genetic variations, which may affect processes like DNA repair or immune response, often face heightened vulnerability. Studies have shown that these interactions can result in significant differences in cancer incidence rates among individuals, highlighting the need for personalized risk assessments.
Additionally, lifestyle changes can serve as powerful modifiers of genetic risk. For instance, individuals with genetic predispositions to smoke-related cancers can reduce their likelihood of developing these conditions by quitting smoking, adopting a healthy diet, and engaging in regular physical activity. Interventions that focus on altering exposure to risk factors can mitigate the impact of genetic predispositions, demonstrating the dynamic relationship between our genetic blueprint and environmental influences. The combination of genetic information and lifestyle changes can pave the way for more effective prevention strategies in managing cancer risk.
The Implications of Genetic Testing for Smokers
Genetic testing has become an integral part of understanding individual health risks, particularly for smokers and those with a family history of smoking-related cancers. This form of testing allows individuals to identify specific genetic markers that indicate a predisposition to certain diseases, including lung cancer and other smoking-related conditions. By understanding one’s genetic makeup, individuals can make informed decisions about their lifestyle and health management.
One practical application of genetic testing for smokers lies in its ability to assess risk levels. If a genetic test reveals a higher susceptibility to smoking-related cancers, it may encourage individuals to reconsider their smoking habits or seek cessation programs. In this way, genetic testing serves not only as a diagnostic tool but also as a motivator for behavioral change. Furthermore, insights gained from genetic analysis can lead to personalized medical screenings, ensuring that smokers receive appropriate monitoring and early intervention if needed.
However, there are inherent limitations associated with genetic testing. The presence of certain genetic markers does not guarantee the development of smoking-related cancers; rather, it indicates an increased risk that can be influenced by various factors, including environmental and lifestyle choices. Additionally, the interpretation of genetic results can be complex, requiring professional guidance to fully understand the implications. This highlights the importance of pre-test and post-test counseling. Health professionals can help smokers navigate the information provided by genetic tests and devise personalized plans aimed at reducing their risk.
While genetic testing is a promising tool for enhancing the understanding of smoking-related cancer risks, it should be regarded as a complement to, rather than a replacement for, conventional health guidelines and preventive measures. In conclusion, through informed discussions and tailored strategies, individuals can harness genetic knowledge to foster healthier living and mitigate potential cancer risks.
Preventive Measures for High-Risk Individuals
Individuals identified as high-risk for smoking-related cancers can adopt several preventive measures to reduce their likelihood of developing such conditions. A pivotal step is embracing lifestyle changes that promote overall health and decrease cancer risk. These modifications often include a balanced diet rich in fruits, vegetables, and whole grains. Evidence suggests that nutrient-dense foods can bolster the immune system and potentially inhibit the growth of cancer cells.
Also read : Rising Norovirus Cases in the US: Understanding Spread and Precautions
Another significant aspect is engaging in regular physical activity. Regular exercise not only aids in maintaining a healthy weight but also improves mental health, which can be beneficial for those attempting to quit smoking. Establishing a consistent exercise routine can lead to reductions in anxiety and stress, which may otherwise trigger relapse into smoking habits.
For high-risk individuals, smoking cessation resources play a vital role in reducing cancer risk. Utilizing nicotine replacement therapy and participating in counseling sessions are effective methods that can significantly improve the chances of quitting smoking successfully. Various programs, including online support groups and helplines, offer tailored resources for those struggling to overcome nicotine addiction. These programs provide not only emotional support but also techniques to cope with cravings and triggers.
Preventive health screenings are another essential strategy for managing cancer risk. Genetic testing can provide insights into individual susceptibility, allowing for personalized screening protocols. Regular health assessments and screenings can facilitate early detection of potential cancerous changes, greatly improving treatment outcomes. Recommendations for screenings vary based on age, medical history, and genetic predisposition, so it is crucial for high-risk individuals to consult healthcare professionals to devise appropriate screening schedules.
Current and Future Research Directions
Research on the genetic connections between smoking and cancer has gained significant momentum in recent years. Investigators are employing advanced genomic techniques to elucidate the specific genetic polymorphisms that may heighten the risk of smoking-related cancers. One pivotal area of exploration is the identification of single nucleotide polymorphisms (SNPs) that correlate with both an increased propensity to smoke and a higher incidence of malignancies such as lung and throat cancers. By understanding these genetic markers, researchers can better assess individual vulnerability to the carcinogenic effects of tobacco.
Moreover, the rapid evolution of gene-editing technologies, particularly CRISPR-Cas9, is paving the way for innovative approaches to studying and potentially mitigating cancer risks associated with smoking. This technology enables researchers to precisely alter DNA sequences, thus offering the capability to investigate the consequences of specific genetic changes. Such studies could yield breakthroughs in not only identifying genetic risk factors but also developing targeted strategies for prevention or treatment of smoking-related lesions.
On the frontier of genomic medicine, there is increasing interest in personalized treatment strategies that consider an individual’s genetic makeup. Tailoring smoking cessation programs and cancer prevention tactics according to genetic profiles could revolutionize healthcare. Ongoing studies aim to integrate genetic screenings within existing public health frameworks, thus allowing for precise risk assessments and more effective interventions. For instance, individuals with specific genetic variants might benefit from tailored counseling or pharmacological support in their efforts to quit smoking.
Finally, large consortiums are collaborating and pooling data from diverse populations to enhance the robustness of research findings. These initiatives aim to capture a more comprehensive understanding of the genetic landscape associated with smoking-related cancers, ultimately guiding more effective public health strategies and interventions. In conclusion, ongoing and future research endeavors are crucial for unraveling the intricate genetic connections that underpin smoking-related cancer risks, thereby potentially transforming prevention and treatment paradigms in oncology.
Summary: The Importance of Personalizing Cancer Prevention
Throughout this discussion, we have explored the intricate relationship between genetic traits and the risk of developing smoking-related cancers. The research reveals that specific DNA markers can significantly influence an individual’s susceptibility to these malignancies, emphasizing the need for a deeper understanding of genetic predispositions. Such insights open avenues for tailoring cancer prevention strategies, aligning them with one’s unique genetic makeup.
The potential of personalized medicine in transforming cancer prevention cannot be overstated. By identifying individuals who possess genetic traits linked to increased cancer risk, healthcare providers can develop customized screening programs and preventive measures. This personalized approach empowers both individuals and healthcare systems to allocate resources more effectively, enhancing the potential for early detection and improved outcomes.
As we move forward, it becomes increasingly clear that conventional one-size-fits-all strategies in cancer prevention may not be adequate for addressing the complexities of cancer. The evidence concerning the DNA traits associated with smoking-related cancers underscores the necessity for a paradigm shift in how we approach prevention and treatment. By integrating genetic insights into public health policies and clinical practices, we can foster a more informed approach to cancer risk management.
Furthermore, understanding the genetic connections to smoking-related cancers not only aids in prevention but can also inform treatment protocols. For example, patients with specific DNA markers might respond more effectively to particular therapies, supporting the overarching goal of enhancing patient care through personalized treatment strategies.
In conclusion, the ongoing research of genetic links to cancer serves as a foundation for developing individualized cancer prevention and treatment plans. By prioritizing the integration of genetic information into healthcare, we stand to make significant strides in combating smoking-related cancers and improving overall public health outcomes.
Breaking News
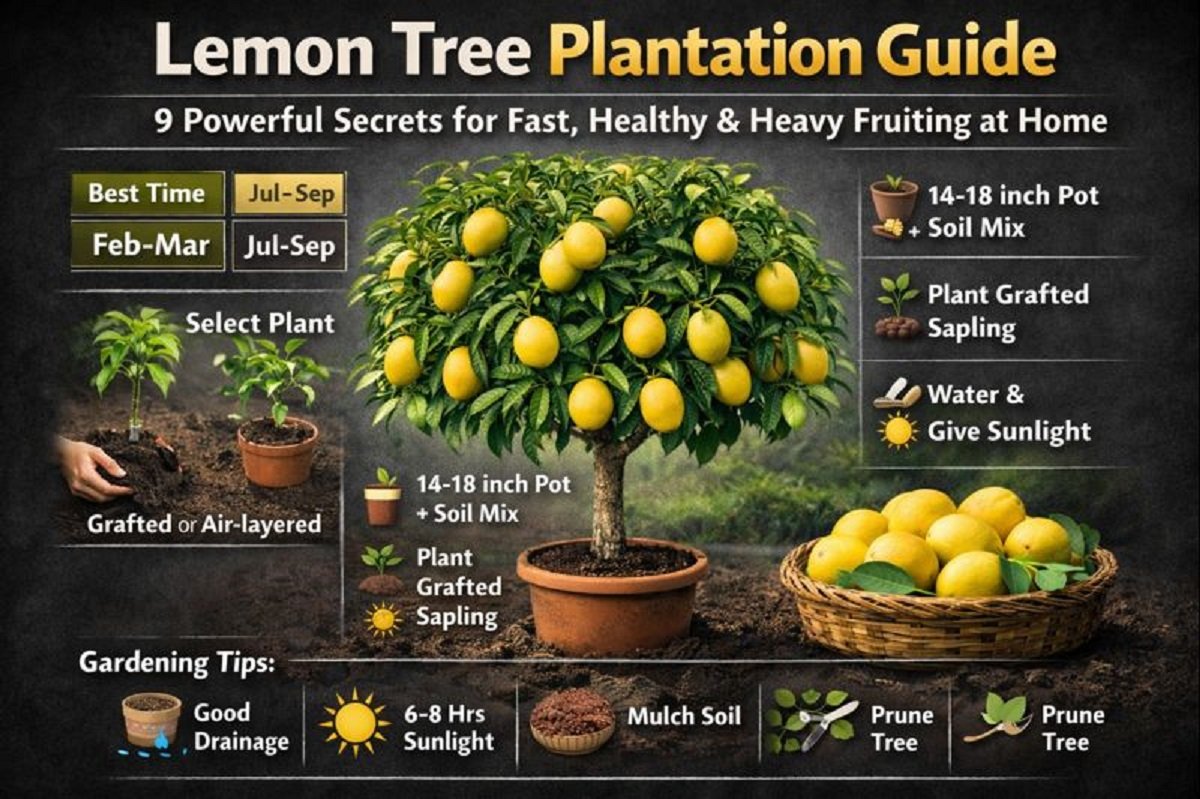
Lemon Tree Plantation Guide-
Contents
Jaipur, Jan.05,2026:Lemon Tree Plantation Guide is emerging as one of the most searched home-gardening topics across India as urban households increasingly turn toward terrace gardening and organic fruit production. Lemon, known for its year-round utility, medicinal value, and high vitamin-C content, is among the easiest fruit trees to grow at home.
This Lemon Tree Plantation Guide explains when, where, and how to plant a lemon tree in pots or soil using scientifically proven methods followed by horticulture experts.
Why Lemon Tree Plantation Is Trending in 2026
According to gardening experts and agricultural advisories, lemon trees are
- Fast-growing
- Suitable for pots
- Productive within 12–18 months
- Ideal for Indian climate
With rising food adulteration concerns, the Lemon Tree Plantation Guide has become a must-read for health-conscious families.
Best Time to Plant
Choosing the correct planting season is critical.
Best Months
- February–March
- July–September
These periods provide optimal temperature and humidity, ensuring faster root establishment and healthy growth.
Ideal Soil & Pot Selection
Soil Requirements
- Well-drained sandy loam soil
- Rich in organic matter
- Slightly acidic to neutral pH
Soil Mix
- 40% cow dung manure or vermicompost
- 10% river sand
- 50% garden soil
Good drainage is a non-negotiable rule in every professional Lemon Tree Plantation Guide.
Choosing the Right Plant
Always buy
- Grafted (कलम किया हुआ) or
- Air-layered lemon plant
Why
- Faster fruiting
- Strong disease resistance
- Uniform fruit quality
Experts from horticulture departments recommend grafted citrus plants for home gardens.
Step-by-Step Plantation Method
Step 1: Pot Preparation
- Use a 14–18 inch pot or grow bag
- Ensure multiple drainage holes
Step 2: Planting the Lemon Tree
- Remove plant gently from nursery bag
- Plant at the same depth as earlier
- Keep the grafting joint above soil level
- Press soil lightly around the roots
Step 3: Initial Watering
- Water immediately after planting
- Keep soil moist, not waterlogged
This phase is crucial in the Lemon Tree Plantation Guide.
Watering Schedule
- Summer: Every 2–3 days
- Winter: Once a week
- Rainy season: Only if soil is dry
Excess water can cause root rot — the most common lemon plant killer.
Sunlight Requirement
Lemon trees need
- 6–8 hours of direct sunlight daily
Balcony, terrace, or open garden locations work best.
Fertilizer & Nutrition Management
Apply organic fertilizers every 1–2 months
- Vermicompost
- Mustard cake solution
- Banana peel compost
- Neem cake
Healthy nutrition ensures continuous flowering and fruiting as explained in this Lemon Tree Plantation Guide.
Pruning & Growth Control Techniques
- Remove dead or diseased branches
- Light pruning promotes new shoots
- Best time: After harvesting
Pruning keeps the lemon tree compact and productive.
Common Problems and Their Solutions
Flower Drop
Causes
- Lack of moisture
- Nutrient deficiency
Solution
- Maintain soil moisture
- Apply organic fertilizer
Yellow Leaves
Cause
- Overwatering or poor drainage
Solution
- Improve soil aeration
Benefits of Growing Lemon Tree at Home
- Fresh chemical-free lemons
- Saves money
- Improves air quality
- Enhances home aesthetics
- Year-round harvesting
Expert Tips for Faster Fruiting
- Mulch soil to retain moisture
- Use Epsom salt occasionally
- Avoid chemical fertilizers
- Rotate pot for uniform sunlight
This Lemon Tree Plantation Guide proves that growing lemons at home is not complicated if the right techniques are followed. With proper timing, soil preparation, sunlight, and organic care, your lemon plant can produce healthy fruits for years.
Breaking News
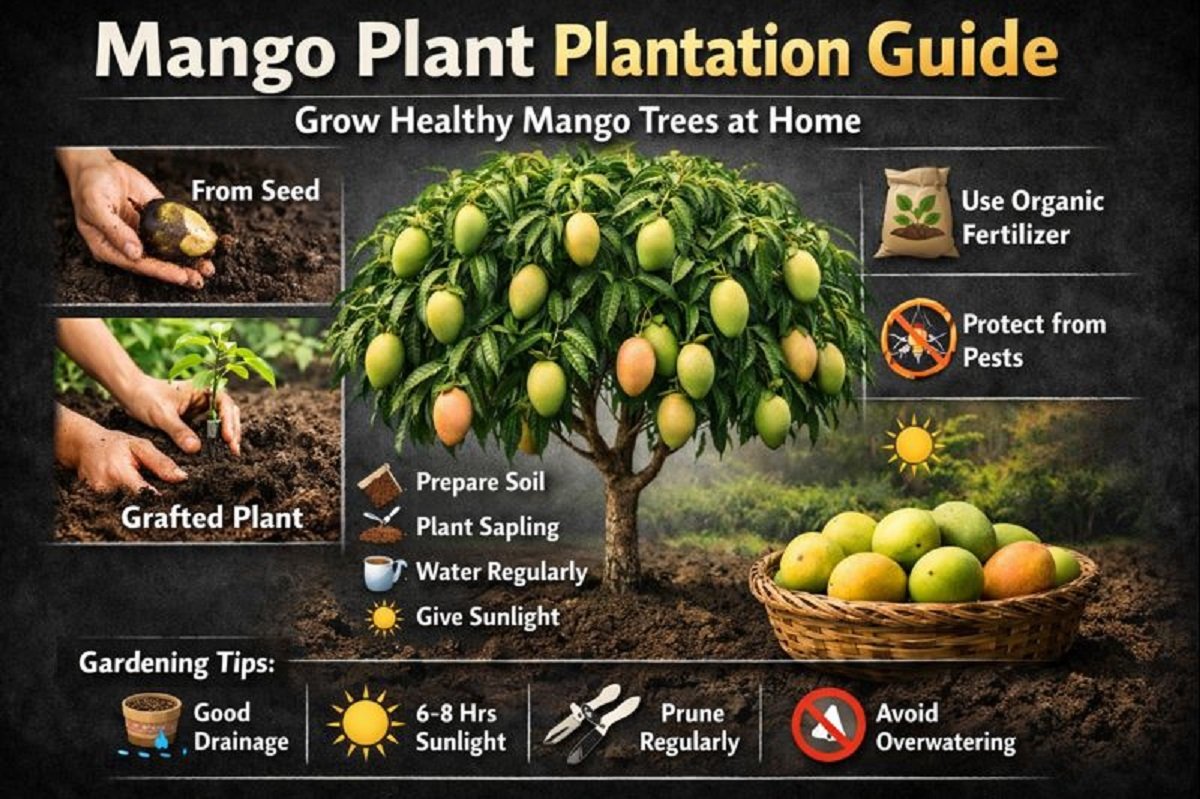
Mango Plant Plantation Guide-
Contents
Jaipur,Jan.05,2026:Mango Plant Plantation Guide is becoming one of the most searched gardening topics in India as more people turn towards home gardening, organic fruits, and sustainable living. Mango, known as the King of Fruits, holds deep cultural, nutritional, and economic value.
Whether you live in a house with a backyard or an apartment with a terrace, this Mango Plant Plantation Guide will help you grow a healthy mango tree using either a seed (गुठली) or a nursery-grown grafted plant.
Why Mango Plantation Is Gaining Popularity
The rising demand for chemical-free fruits and the joy of growing food at home have made mango plantation a trending topic. According to horticulture experts and agricultural advisories, mango trees are hardy, long-living, and highly rewarding when planted correctly.
This Mango Plant Plantation Guide explains simple yet powerful methods that even beginners can follow.
Best Climate & Soil
- Climate: Tropical to subtropical
- Temperature: 24°C – 35°C
- Soil Type: Well-drained loamy or sandy loam
- Soil pH: 5.5 – 7.5
Good drainage is critical. Waterlogged soil can damage mango roots permanently.
Mango Plant Plantation Guide Using Seed (गुठली से पौधा लगाना)
Growing mango from seed is economical and educational, though it takes more time to bear fruit.
Step 1: Seed Preparation
- Wash the mango stone thoroughly
- Dry it for 1–2 days
- Carefully break the outer shell
- Extract the inner seed
- Wrap it in a moist cloth for germination
This step is crucial in the Mango Plant Plantation Guide.
Step 2: Pot & Soil Preparation
- Use a 12–18 inch pot with drainage holes
- Mix:
- Garden soil
- Compost
- Well-decomposed cow dung manure
Healthy soil is the foundation of successful mango growth.
Step 3: Planting the Seed
- Plant the germinated seed 2 inches deep
- Cover lightly with soil
- Water gently
Step 4: Early Care
- Keep the pot in partial shade
- Maintain moisture, not excess water
- Once the plant grows stronger, shift it to a 45 cm deep pot or garden soil
This stage defines success in the Mango Plant Plantation Guide.
Mango Plant Plantation Guide Using Nursery (Grafted) Plant
For faster fruiting, experts recommend grafted plants.
Step 1: Selecting the Right Plant
- Choose a healthy, disease-free grafted mango plant
- Preferred varieties: Alphonso, Dasheri, Langra, Kesar
Step 2: Pit Preparation
- Dig a pit of 1x1x1 feet
- Best done during summer
- Mix excavated soil with:
- Compost
- Cow dung manure
- Trichoderma (bio-fungicide)
Step 3: Plantation
- Place plant gently without damaging roots
- Fill pit with prepared soil
- Press soil lightly around base
Step 4: Watering & Shade
- Water immediately
- Provide shade for initial days
- Gradually expose to sunlight
This method is widely recommended in professional Mango Plant Plantation Guide manuals.
Watering Schedule
- Initial stage: Water every 2–3 days
- Established plants: Once a week
- Avoid waterlogging
Overwatering is one of the biggest mistakes in mango cultivation.
Sunlight & Location
- Young plants need protection from harsh sunlight
- Mature mango trees need 6–8 hours of direct sunlight daily
Sun exposure directly affects flowering and fruit quality.
Fertilizer & Nutrition Management
Apply organic manure during
- July–August
- September
Recommended nutrients:
- Compost
- Vermicompost
- Neem cake
Balanced nutrition is a core principle of any Mango Plant Plantation Guide.
Protection From Pests & Animals
- Use fencing or bamboo support
- Protect young plants from goats and cattle
- Apply neem oil spray for pest control
Common Mistakes to Avoid
- Excess watering
- Poor drainage
- Ignoring sunlight needs
- Planting in very small containers
Avoiding these mistakes ensures success with this Mango Plant Plantation Guide.
Benefits of Growing Mango at Home
- Chemical-free fruits
- Long-term investment
- Environmental benefits
- Shade and greenery
- Emotional satisfaction
Expert Gardening Tips
- Mulch soil to retain moisture
- Prune lightly after 2–3 years
- Use organic pesticides only
This Mango Plant Plantation Guide is designed to help beginners and gardening enthusiasts grow mango trees successfully at home. With patience, proper care, and organic practices, your mango tree will thrive for decades and reward you with delicious fruits.
Breaking News
Chyawanprash Health Benefits-

Contents
Jaipur,Jan.02,2026:Chyawanprash Health Benefits have made this ancient Ayurvedic formulation an inseparable part of Indian households. From children to the elderly, millions rely on it daily to strengthen immunity, enhance energy levels, and protect the body from seasonal illnesses.
In today’s world of rising pollution, frequent infections, and stressful lifestyles, people are actively searching for natural and preventive health solutions. This is where Dabur Chyawanprash Health Benefits stand out—offering a time-tested, research-backed approach to holistic wellness.
A Timeless Ayurvedic Rasayana
Chyawanprash is one of the oldest known Ayurvedic Rasayana (rejuvenation tonic), mentioned in classical texts like the Charaka Samhita and Rigveda. Traditionally prepared to restore youthfulness and vitality, it was originally formulated for sage Chyawan to regain strength and longevity.
Ayurvedic scholars describe it as an “Ageless Wonder” due to its ability to nourish body tissues, strengthen immunity, and slow down ageing.
Learn more about Rasayana therapy from the Ministry of AYUSH
Health Benefits Backed by Ayurveda & Science
Unlike many modern supplements, Dabur Chyawanprash Health Benefits are rooted in both ancient wisdom and modern scientific validation. Dabur has combined centuries-old Ayurvedic knowledge with contemporary research, quality control, and innovation.
Each spoon contains a powerful blend of Amla (Indian Gooseberry), natural antioxidants, essential minerals, and over 40 Ayurvedic herbs.
The Core of Chyawanprash Health Benefits
One of the most trusted Dabur Chyawanprash Health Benefits is its powerful effect on immunity.
How It Works
- Enhances Immunoglobulin G (IgG) and IgM, which protect against infections
- Helps regulate IgE, reducing allergic reactions
- Lowers histamine levels, easing respiratory and seasonal allergies
Scientific studies indicate that regular consumption improves the body’s immune response against pathogens.
How Chyawanprash Boosts Energy, Stamina, and Vitality
Low energy and fatigue are common problems across age groups. Dabur Chyawanprash Health Benefits include natural energy enhancement without artificial stimulants.
Key Advantages
- Improves oxygen utilization
- Enhances metabolic efficiency
- Supports muscle and tissue nourishment
- Reduces tiredness and weakness
This makes it ideal for students, working professionals, athletes, and senior citizens.
The Ayurvedic Advantage
According to Ayurveda, good health depends on the balance of Vata, Pitta, and Kapha doshas.
Dabur Chyawanprash Health Benefits include
- Calming excess Vata (reduces weakness and anxiety)
- Regulating Pitta (supports digestion and metabolism)
- Strengthening Kapha (boosts immunity and endurance)
This tri-dosha balance ensures overall physical and mental harmony.
Anti-Ageing and Antioxidant Properties Explained
Ageing begins at the cellular level. Dabur Chyawanprash Health Benefits include protection against oxidative stress caused by free radicals.
Antioxidant Power
- High polyphenols and gallic acid from Amla
- Flavonoids and tannins for cellular repair
- Supports skin health, memory, and organ function
These compounds slow down premature ageing and promote youthful vitality.
The Power of Amla and 40+ Herbs in Dabur Chyawanprash
Amla forms the backbone of Dabur Chyawanprash, providing natural Vitamin C in its most stable form.
Key Ingredients Include
- Amla – Immunity and antioxidant powerhouse
- Pippali – Respiratory support
- Ashwagandha – Stress relief and stamina
- Giloy – Detox and immune modulation
- Cow Ghee & Sesame Oil – Nutrient absorption enhancers
Together, they amplify Dabur Chyawanprash Health Benefits manifold.
Scientific Research Supporting Chyawanprash Health Benefits
Experimental studies reveal that Chyawanprash
- Reduces allergic responses
- Lowers serum IgE levels
- Suppresses histamine release
- Improves long-term immune memory
Such findings validate Ayurveda through modern biomedical research.
Allergy Protection and Respiratory Wellness
Seasonal cough, asthma, and breathing issues worsen in winter. Chyawanprash Health Benefits extend to respiratory health by:
- Strengthening lung tissues
- Reducing inflammation
- Improving airflow and oxygen exchange
It acts as a protective shield against pollution-related respiratory problems.
Why Chyawanprash Is Different From Other Supplements
Unlike synthetic immunity boosters, Dabur Chyawanprash
- Is natural and preservative-free
- Works holistically, not symptomatically
- Is safe for long-term daily use
- Is backed by over 135 years of Ayurvedic expertise
This makes Dabur Chyawanprash Health Benefits truly sustainable.
How to Consume Chyawanprash for Maximum Health Benefits
Recommended Dosage
- Adults: 1–2 teaspoons daily
- Children: ½–1 teaspoon daily
Consume with warm milk or water for better absorption.
Who Should Take Chyawanprash
- Children with low immunity
- Adults facing fatigue and stress
- Elderly individuals
- People prone to allergies
- Anyone seeking natural wellness
Chyawanprash in Modern Indian Lifestyle
In today’s fast-paced life, Dabur Chyawanprash Health Benefits offer a simple daily ritual for long-term health—bridging ancient wisdom with modern living.
Why Chyawanprash Remains India’s Daily Health Shield
Chyawanprash Health Benefits go far beyond immunity. They represent India’s holistic approach to health—natural, preventive, and deeply rooted in tradition.
From boosting energy and protecting against diseases to slowing ageing and enhancing vitality, Chyawanprash continues to be a trusted wellness companion for every Indian household.
Breaking News
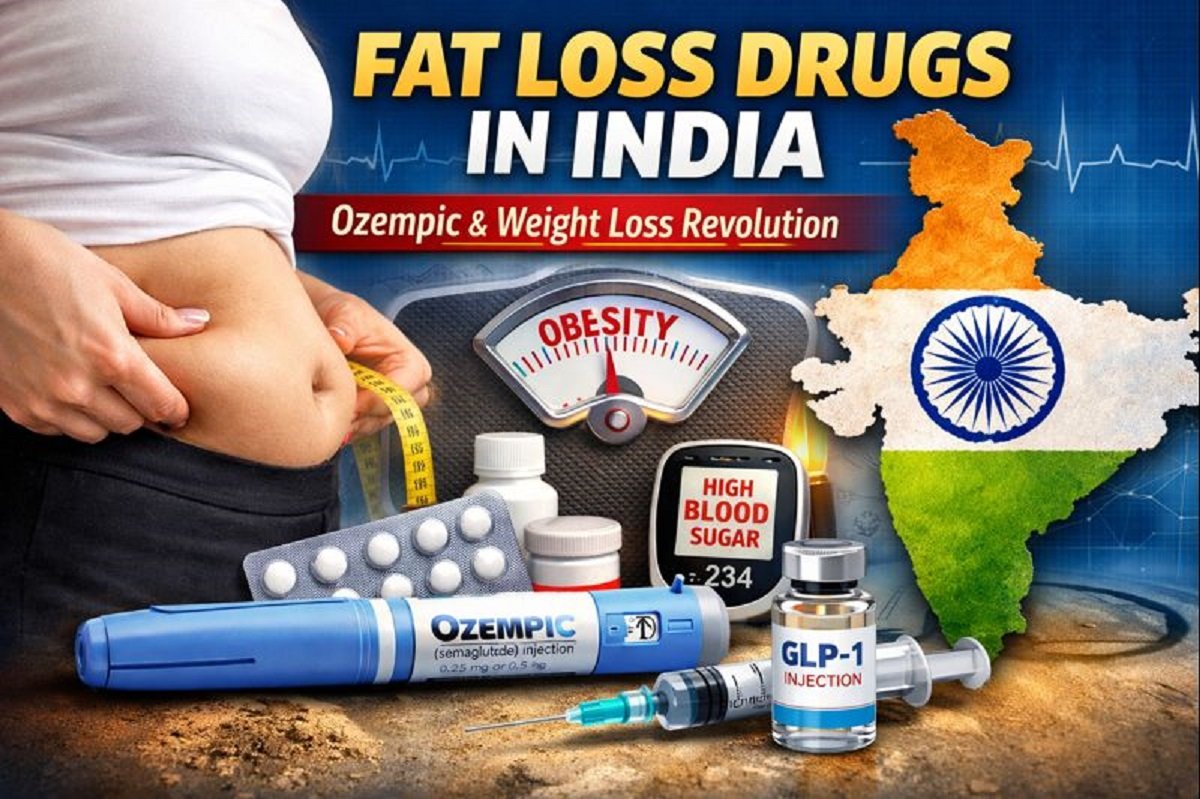
Fat Loss Drugs in India are gaining massive attention after Ozempic’s launch-
Contents
Jaipur, Dec.17,2025:Fat Loss Drugs in India have become one of the most discussed topics in the health and pharmaceutical space after the official launch of Ozempic by Danish drugmaker Novo Nordisk. Originally developed to treat Type-2 diabetes, this injectable medicine is now being widely talked about for its remarkable weight loss effects.
From celebrities to medical experts, everyone seems to be debating whether these drugs are a breakthrough solution for obesity or a risky shortcut. With India facing a twin epidemic of diabetes and obesity, the timing of Ozempic’s entry could not be more critical.
What Are Fat Loss Drugs in India
Fat Loss Drugs in India primarily refer to a new class of medicines based on GLP-1 (Glucagon-Like Peptide-1) receptor agonists. These drugs were initially created to help people manage blood sugar levels but later showed strong results in reducing appetite and body weight.
Popular GLP-1 based drugs include
- Ozempic (Semaglutide)
- Wegovy
- Rybelsus (oral version)
- Mounjaro (Tirzepatide – not yet widely available in India)
These medicines are taken either as weekly injections or daily pills, under medical supervision.
A Game-Changer
The launch of Ozempic has pushed Fat Loss Drugs in India into the mainstream conversation. Novo Nordisk introduced Ozempic as a Type-2 diabetes treatment, but global studies and real-world usage revealed its strong impact on fat loss and appetite control.
According to multiple international reports, patients using Ozempic experienced
- Reduced hunger
- Slower digestion
- Lower calorie intake
- Significant weight reduction over months
This has made Ozempic one of the most talked-about drugs worldwide.
How GLP-1 Drugs Work in the Human Body
To understand Fat Loss Drugs in India, it is important to understand how GLP-1 hormones function.
GLP-1 is a natural hormone released by the intestines after eating food. It helps the body by
- Increasing insulin secretion
- Slowing stomach emptying
- Reducing hunger signals to the brain
- Controlling blood sugar levels
GLP-1 based drugs mimic this hormone, making the body feel full faster and for longer durations. As a result, calorie intake reduces naturally, leading to gradual and sustained fat loss.
Fat Loss Drugs in India and the Diabetes Crisis
India is often called the diabetes capital of the world. A 2023 study published in The Lancet Diabetes & Endocrinology revealed that over 101 million people in India are living with diabetes, with the majority suffering from Type-2 diabetes.
Despite awareness campaigns under the National Health Mission (NHM), diabetes remains a major public health challenge.
Fat Loss Drugs in India are now being seen as a dual-purpose solution
- Managing diabetes
- Tackling obesity, which is a major risk factor
Scientific Evidence Behind Ozempic and Weight Loss
Multiple international clinical trials have demonstrated the effectiveness of semaglutide-based drugs.
Key findings include
- Average weight loss of 10–15% over one year
- Improved insulin sensitivity
- Reduced cardiovascular risk
A study published in The New England Journal of Medicine confirmed that patients using semaglutide lost significantly more weight compared to placebo groups.
Benefits of Fat Loss Drugs in India
The growing popularity of Fat Loss Drugs in India is driven by several benefits
Key Advantages
- Clinically proven weight loss
- Better blood sugar control
- Reduced risk of heart disease
- Improved metabolic health
- Appetite regulation without extreme dieting
For patients struggling with obesity and diabetes together, these drugs offer a medical alternative to bariatric surgery.
Risks, Side Effects, and Medical Warnings
Despite the hype, Fat Loss Drugs in India are not risk-free.
Common side effects include
- Nausea
- Vomiting
- Diarrhea
- Constipation
- Fatigue
Serious but rare risks
- Pancreatitis
- Gallbladder issues
- Thyroid tumors (observed in animal studies)
Doctors strongly advise against self-medication. These drugs should only be used under professional medical supervision.
Who Should and Should Not Use These Drugs
Fat Loss Drugs in India are generally prescribed for
- Adults with Type-2 diabetes
- Individuals with BMI above 30
- Patients with obesity-related health conditions
Not recommended for
- Pregnant or breastfeeding women
- People with thyroid cancer history
- Patients with severe gastrointestinal disorders
Medical screening is essential before starting treatment.
Cost, Availability, and Accessibility in India
One of the biggest concerns around Fat Loss Drugs in India is affordability.
Estimated monthly cost
- ₹8,000 to ₹15,000 (varies by dosage)
Currently, these drugs are not covered under most government schemes, making them inaccessible for a large section of the population.
Government Health Programs vs Ground Reality
While the Ministry of Health promotes lifestyle changes under NHM, the growing burden of diabetes and obesity highlights a gap between policy and ground-level implementation.
Experts believe medicines alone cannot solve the problem without
- Nutrition education
- Physical activity promotion
- Early screening programs
Expert Opinions on Fat Loss Drugs in India
Health experts caution against calling these drugs “miracle solutions.”
According to endocrinologists:
“GLP-1 drugs are effective medical tools, not cosmetic weight loss shortcuts.”
Long-term lifestyle changes remain essential for sustainable health outcomes.
Ethical and Social Concerns Around Weight Loss Drugs
The rise of Fat Loss Drugs in India has sparked ethical debates:
- Are these drugs being misused for cosmetic weight loss?
- Will shortages affect diabetic patients?
- Is society promoting medication over healthy habits?
These concerns need urgent regulatory attention.
The Future of Fat Loss Drugs in India
The future looks promising yet cautious. Pharmaceutical companies are investing heavily in next-generation GLP-1 drugs, while Indian regulators are closely monitoring usage patterns.
Experts predict
- Wider availability
- Possible price reductions
- Stricter prescription guidelines
Miracle Cure or Medical Tool
Fat Loss Drugs in India represent a significant medical advancement in tackling diabetes and obesity. However, they are not magic bullets. Used responsibly, under medical guidance, they can improve lives. Misused, they could create new health risks.
As India battles a growing lifestyle disease crisis, the real solution lies in a balanced approach combining medicine, awareness, and healthy living.
We do not provide advice for any medicine; this is only for informational purposes.
Breaking News
hidden sugar in everyday foods is raising your diabetes and heart-disease risk –

Contents
Jaipur, Nov.08,2025:hidden sugar is a term you may have heard casually, but it deserves serious attention. Despite our best efforts to eat healthily, we may unknowingly be consuming large amounts of sugar — not just the lumps of white table sugar, but the sugar that is already embedded in the foods we eat every day. This silent sugar exposure can drive weight gain, type 2 diabetes, heart disease, and other chronic illnesses. With escalating rates of obesity and diabetes globally, it’s time to pull back the curtain and expose the hidden sugar in everyday foods.
In this article we’ll define what hidden sugar really means, show you where it hides, explain how it harms health, review the global trend, and give you actionable tools to detect and reduce it.
What is hidden sugar
By “hidden sugar” we mean sugar that is not obviously present (like a candy bar) but rather appears in everyday foods and drinks that appear healthy, savoury, or innocent. The sugar may be added by manufacturers (so-called “added sugars” or “free sugars”) or may be naturally present but in a form that leads to a rapid blood-sugar spike.
According to the World Health Organization (WHO), “free sugars” include monosaccharides and disaccharides added to foods and beverages by the manufacturer, cook or consumer, and sugars naturally present in honey, syrups, fruit juices and fruit juice concentrates.
Hidden sugar is dangerous because it adds to total sugar intake without you realising it. Many health-organisations warn that the modern diet’s sugar content is far higher than in prior generations, and that much of this comes from processed, packaged or prepared foods. For example, research shows that ultra-processed foods — which tend to contain added sugars, among other additives — are linked to higher risks of type 2 diabetes.
Thus, hidden sugar isn’t just a trivia item — it’s a significant public-health issue.
Everyday foods where hidden sugar lurks
Dairy & yoghurt
Many people assume yoghurt is a health-food. But flavoured yoghurts can contain significant added sugar. The Centres for Disease Control and Prevention (CDC) warns that packaged yoghurts and dairy products may have high amounts of added sugars.
For example, a “fruit-on-the-bottom” cup may have sugar levels comparable to a dessert. Because you expect yoghurt to be healthy, you may not account for that sugar in your daily total.
Bread, buns & bakery items
Bread and bakery items may seem low-risk, but many commercial breads contain sweeteners or sugar to improve texture, aid fermentation, or prolong shelf life. A recent Indian news article flagged that breads and buns often contain more sugar than consumers expect.
Thus something as “innocent” as your sandwich bread may contribute to your hidden sugar load.
Condiments, sauces and “savory” processed foods
One of the biggest culprits for hidden sugar is savoury foods that you wouldn’t suspect: ketchup, pasta sauce, salad dressings, sausages, processed meats. The CDC specifically lists condiments and sauces as common sneaky sources of added sugar.
For example, a single tablespoon of ketchup may already add 3-4 g of sugar.
Drinks, juices and smoothies
Bottled juices, smoothies, energy drinks, flavoured milks — these are classic hidden sugar sources. Even “100 % fruit juice” can contain a high free-sugar load, because fibre is removed during juicing and the sugars act like free sugars.
Also, when you drink sugar rather than eating food, the sugars can be absorbed more rapidly, spiking blood sugar and contributing to metabolic risk.
Ultra-processed snacks and cereals
Breakfast cereals, granola bars, snack foods often carry added sugars under multiple names. Many items marketed as “healthy” may in fact contain sugar as a primary ingredient. The Johns Hopkins Medicine site warns that “whole-grain” or “vitamin-fortified” do not guarantee low sugar.
Artificial intelligence research shows that across many countries, packaged foods often fail to meet carbohydrate-quality benchmarks because of high free-sugar content.
obesity, diabetes, heart disease, and more
When you repeatedly consume hidden sugar beyond what your body can handle, multiple pathways lead to harm.
- Excess sugar contributes to weight gain because it adds calories, often without making you feel full. The WHO says keeping free sugar intake under 10% of total energy reduces risk of overweight and obesity.
- As weight increases, the risk of type 2 diabetes rises. Also, high sugar intake independently can reduce insulin sensitivity.
- Heart disease: hidden sugar plays a role in high blood pressure, inflammation, fatty-liver and cardiovascular risk independent of cholesterol. For example, a recent cardiologist statement claimed sugar may damage the heart more than cholesterol by raising risk up to 21%.
- Ultra-processed food consumption (which usually implies high added sugar) is linked to increased type 2 diabetes risk.
In sum, hidden sugar is not simply “extra sweetness” — it’s an insidious contributor to chronic disease.
rising sugar consumption and the toll on health
Global dietary patterns have changed dramatically in recent decades: processed foods, sugary drinks, high-calorie snacks, and hidden sugar infiltration are widespread. According to recent reporting-
- The WHO guideline suggests reducing free sugars to less than 10% of total energy intake, and ideally below 5% for additional benefits.
- A recent article noted that hidden sugars are “silently increasing health risks like obesity and diabetes” in India, urging awareness of routine foods.
- A machine-learning study found varying compliance across countries in packaged foods meeting carbohydrate-quality standards; some countries had as low as ~9.8% of foods meeting targets.
Thus, hidden sugar is a global phenomenon with local consequences — especially in nations undergoing nutritional transition (such as India, where packaged foods and snacks are growing rapidly).
How to detect and reduce hidden sugar intake
Read labels and watch ingredient lists
One of the first steps is label literacy. The CDC says reading nutrition labels to assess total sugars and added sugars is vital.
Tips-
- Look at “added sugars” or “free sugars” if listed.
- Check the ingredient list: if sugar (or corn syrup, dextrose, fructose, honey, agave nectar) is among the first few ingredients, the product likely has high added sugar.
- Be sceptical of claims like “low-fat” or “whole grain” without checking sugar content.
- Watch serving sizes: what looks small may hide large sugar loads.
Choose whole foods and cook at home
One sure way to avoid hidden sugar- favour unprocessed or minimally processed foods. Fresh vegetables, whole grains, legumes, plain dairy, unflavoured milk/yoghurt. Make your own sauces, dressings, breads. When you control ingredients, you avoid the surprises.
Understand added vs natural sugars
Not all sugars are equal. Sugars naturally present in whole fruits and milk are less problematic because fibre, fat and structure slow absorption. The problem arises when sugars are “free” or added, causing rapid absorption and higher metabolic impact.
Practical switching tips
- Swap flavoured yoghurt for plain yoghurt + fresh fruit.
- Choose breads with minimal added sugar (check label).
- Replace sweetened condiments with homemade versions: e.g., tomato-puree + herbs instead of packaged ketchup.
- Choose water, unsweetened tea/coffee instead of sugary drinks or juices.
- Eat breakfast cereal only if sugar < 5 g/serving or switch to oatmeal with nuts and seeds.
- When buying snacks, pick those with short ingredient lists and no sugar synonyms (corn syrup, maltose, etc.).
body mass index (BMI), health equity & vulnerable groups
While the hidden sugar issue is universal, there are special angles to consider. The common measure of overweight/obesity is the body mass index (BMI), but this measure has limitations: it does not account for body-fat distribution, muscle mass, age, ethnicity. In some ethnic groups (e.g., South Asians) the risk of type 2 diabetes or heart disease may be higher even at lower BMI levels. Thus, relying solely on BMI may mask real risk.
Moreover, hidden sugar harms are affected by social determinants: access to fresh whole foods, education about labels, marketing of processed foods, and socio-economic status. Countries in transition (with rising incomes and shifts to processed-food diets) face steep increases in overweight and diabetes. For example, some forecasts indicate by 2050 over half of adults globally may be overweight or obese if current trends continue.
Therefore the hidden sugar narrative must also include equity: those with fewer resources may be disproportionately impacted.
hidden sugar is more than an inconvenient ingredient — it’s a stealth driver of chronic disease risk. The good news is: awareness and action work. By understanding where sugar hides, reading labels, favouring whole foods, cooking at home, and making smarter swaps, you can significantly reduce your exposure. Given the global rise of obesity, type 2 diabetes and heart disease, uncovering the hidden sugar in your diet is a powerful step toward reclaiming your health.
Breaking News
Back Pain Breast Cancer link revealed — why persistent unexplained back pain may be an early sign and when you must seek medical help-

Contents
Jaipur, Nov.08,2025:Back pain breast cancer might sound alarmist, yet it is a phrase worth remembering. When back pain is persistent, unexplained, grows worse at night or is accompanied by other subtle symptoms—what you think is just “muscle strain” could sometimes signal something far more serious, such as the early stages of breast cancer or its spread. Recent articles highlight that while back pain is rarely due to cancer, in certain instances it may reflect a diagnosis of breast cancer that has progressed or metastasised-
Understanding when back pain is simply benign and when it could be an early warning of breast cancer can empower women to act—and potentially change outcomes.
What the research says on back pain breast cancer
The rarity but significance
Medical research shows that, in the majority of cases, back pain is not caused by cancer. For instance, a review by Dana‑Farber Cancer Institute noted that although 39 % of adults experience back pain each year, the cause is rarely cancer. That said, cases exist where breast cancer that has spread (metastasised) to bones—especially the spine—can cause back pain.
Back pain as a sign of advanced breast cancer
According to a Medical News Today article
“Back pain is more likely to be a symptom of advanced (metastatic or stage 4) breast cancer, which means the cancer has spread to other parts of the body.”
And the UK’s Cancer Research UK confirms bone pain, including back pain, is a common symptom when breast cancer has spread to the bones.
Thus, while back pain breast cancer is not typical in early, localised breast cancer, it can be a red flag of advanced spread.
how it happens
When breast cancer cells spread to the bones of the spine, they weaken bone structure, create pressure or fractures, and irritate nearby nerves — all of which can lead to back pain. Some treatments for breast cancer (like hormonal therapy, chemotherapy) can also cause spine or joint-related pain, adding to confusion.
typical back pain vs back pain breast cancer
Since back pain is extremely common, the challenge is distinguishing benign causes from possible signs of breast cancer. Here are key differentiators-
Typical muscular/back pain features
- Related to movement, posture, lifting, or a sudden strain.
- Improves with rest, stretching, pain-relief measures, or behavioural changes (e.g., better mattress, correct posture).
- Often variable in intensity and location; may improve with time.
Back pain breast cancer features
- Persistent for weeks without clear cause (i.e., not from lifting, posture, pressure) and not improving.
- Occurs or worsens at night, or when lying down.
- May be localised to spine, ribs, pelvis or hips — where breast cancer often spreads.
- Accompanied by other systemic symptoms: unexplained weight loss, fatigue, loss of appetite, swelling, numbness or tingling in limbs.
- Occurs in context of known breast cancer or breast symptoms (lump, discharge, skin change), though sometimes before a breast lesion is detected.
By being aware of these differences, women can be alert to when back pain goes beyond the usual.
Warning signs and red flags of back pain breast cancer
Here are five powerful warning signs every woman should know under the umbrella of back pain breast cancer-
Persistent and Unexplained Back Pain
If your back pain is of unknown origin (no clear injury, no posture cause) and lasts beyond several weeks without improvement, this is a signal. Unlike typical muscle pain, which may ease with rest or therapy, back pain breast cancer-related often continues or worsens.
Night-Time or Resting Pain
Back pain that worsens at night or while lying down—especially when you wake with it or cannot get comfortable—is concerning for possible spinal involvement.
Pain that Spreads or Is Associated with Other Symptoms
If the pain radiates to hips, thighs, ribs or is accompanied by numbness or weakness in limbs—alongside signs like fatigue, weight loss or appetite reduction—it could be more than a strained muscle. The UK Cancer Research site emphasises that bone-spread symptoms often include pain and general signs of decline.
Existing Breast Symptoms + Back Pain
If you already have breast symptoms (lump, discharge, skin change) and back pain arises or persists, you should not ignore it. The link between breast issues and back pain must prompt evaluation.
Known History of Breast Cancer
For women who have had breast cancer before, new or worsening back pain must be evaluated promptly—it may indicate recurrence or metastasis. Even treatments themselves (chemo, hormone therapy) can contribute to back pain, but an evaluation is still warranted.
Why early detection matters for back pain breast cancer
Improved outcomes
When breast cancer—especially one that has begun to spread—is detected early, treatment options widen, and outcomes improve significantly. Although back pain in itself doesn’t guarantee cancer, treating when caught early (for any breast cancer) offers better prognosis.
Avoiding irreversible damage
Bone metastasis, particularly in the spine, can lead to fractures, spinal cord compression, nerve damage, paralysis, or severe pain. For instance, Cancer Research UK says spinal cord compression is an emergency and back pain may be its first symptom.
Distinguishing treatable causes
If back pain is due to benign causes, quick evaluation confirms that and you can return to normal life with peace of mind. If it’s due to breast cancer or spread, early action helps. As a recent article noted:
“Back pain linked to breast cancer: Early warning signs you should never ignore.”
Thus, vigilance over back pain breast cancer isn’t fear-mongering: it is responsible health awareness.
Practical steps if you suspect back pain breast cancer
Here’s what to do if you have back pain and are concerned about its link to breast cancer
Seek medical evaluation
Don’t delay. Tell your doctor that the pain is persistent and unexplained. Provide details: when it started, where exactly, how it feels, what worsens it, whether you have other symptoms, and any breast symptoms/history.
Request appropriate investigations
Depending on your situation, investigations may include:
- Mammogram or breast ultrasound (if you haven’t had one).
- MRI or CT scan of the spine or bones if bone metastasis is suspected.
- Bone scan or PET scan to assess spread to bones or other organs. Medical News Today outlines this process.
Pay attention to self-exams and screening
For all women, regular breast self-exams and screening mammograms (per local guidelines) are critical. If you detect any breast changes (lumps, skin thickening, discharge, nipple inversion) and persistent back pain, act swiftly.
Manage lifestyle and risk factors
While back pain breast cancer may be rare, general breast health helps. Maintain healthy weight, reduce alcohol, stay active, eat a balanced diet, avoid smoking, and maintain a healthy posture and spine-care to reduce benign back pain.
Don’t ignore other signs
Besides back pain, unusual fatigue, unexplained weight loss, bone pain elsewhere, or neurological signs (numbness, weakness) necessitate urgent medical review.
- Back pain breast cancer is rare, but it is a possible sign when back pain is persistent, unexplained and accompanied by other symptoms.
- The probability of back pain being related to breast cancer increases when there are breast symptoms/history or when the pain occurs at night, worsens, or is located in spine/bone zones.
- Early detection of any breast cancer—even when presenting atypically through back pain—improves outcomes and reduces risk of severe complications.
- Regular screening and attunement to your body’s signals are vital. If something feels “off” with your back and you don’t have a clear explanation, don’t dismiss it as mere fatigue or posture-error.
- Always consult a healthcare professional rather than diagnosing yourself.
Back pain breast cancer may not be the most common phrase you’ll hear, but it’s one worth remembering. If you are a woman experiencing back pain that doesn’t resolve, especially alongside any breast symptoms or risk factors, being proactive could make all the difference. Don’t wait—listen to your body, trust your instincts, and seek help when something doesn’t feel right. Early action is powerful.
Breaking News
Air Pollution Organ Damage is more than just lung disease—
Contents
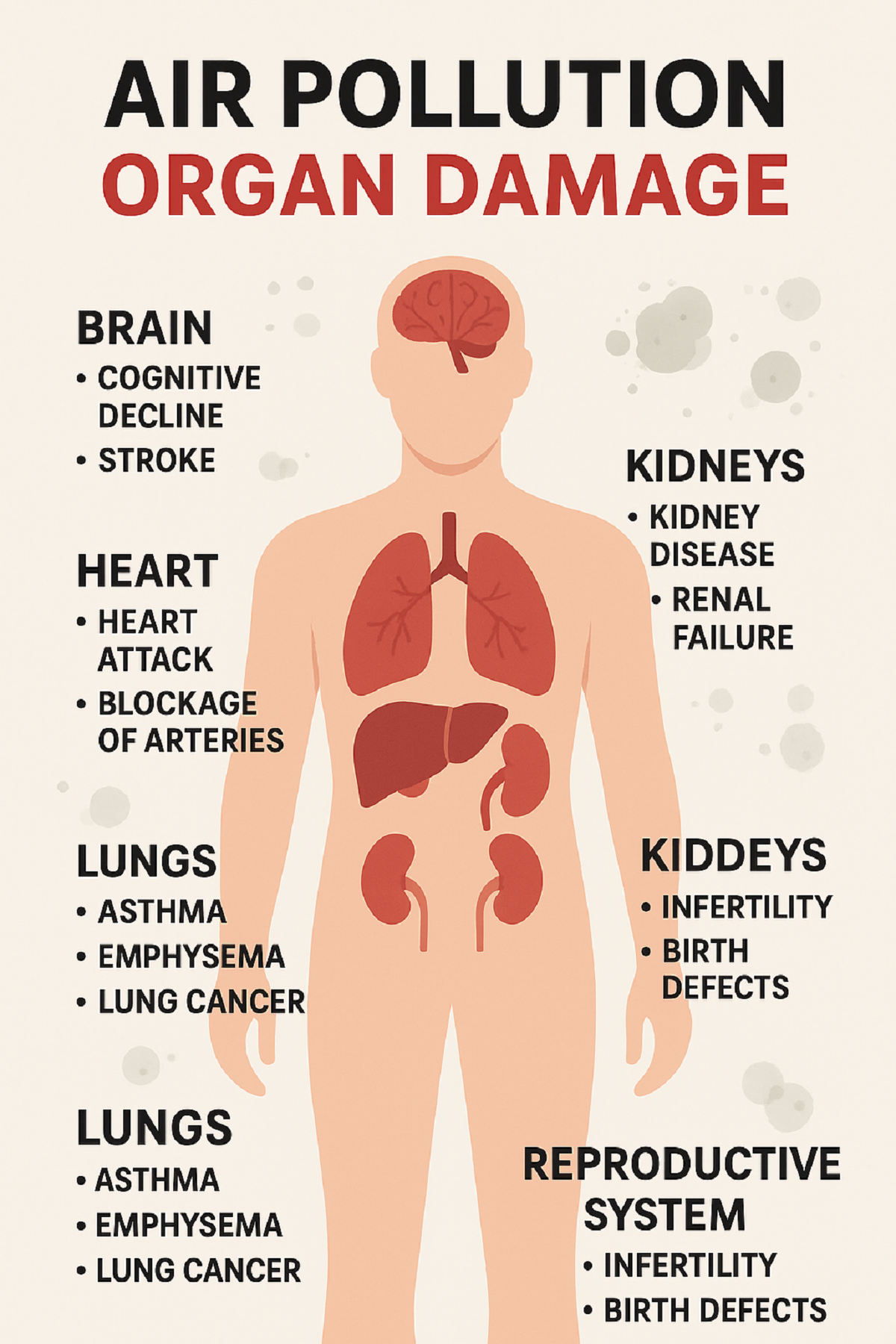
New Delhi, Nov.06,2025:When we talk of air pollution, the first thought is often smog, wheezing, or lung problems. But the term Air Pollution Organ Damage captures a wider reality: fine and ultra-fine particles (like PM2.5, PM10, even <0.1 microns), gases (NO₂, CO, SO₂) and toxic chemical compounds infiltrate the body, travel via the bloodstream, and damage multiple organs. Experts now warn that what we breathe in the winter months of Delhi isn’t just making us cough—it’s harming our heart, brain, kidneys and even our reproductive health-
The stakes are huge. According to one article, nearly 15 % of all deaths in Delhi in 2023 were linked to air pollution. That underlines how Air Pollution Organ Damage shifts the conversation from a seasonal nuisance to a full-scale public health emergency.
The science behind how polluted air harms organs
Particulates, nano-particles & bloodstream entry
Particles with aerodynamic diameter less than 2.5 microns (PM2.5) can reach deep into the alveoli of the lungs; even ultrafine particles (<0.1 microns) can penetrate the alveolar–capillary barrier, enter the bloodstream and move to organs. As one doctor described: “Fine particles … not only reach the lungs they can cross into the bloodstream and travel to all parts of the body.”
Systemic inflammation & oxidative stress
Once in circulation, these particles trigger chronic inflammation and oxidative stress. The body’s immune response remains persistently activated, causing damage to blood vessels, tissues and organs over time. According to research from India: “air pollution is worsening anaemia, hypertension, diabetes, cholesterol levels and mental health” alongside more traditional lung impacts.
Mechanisms of organ damage
- Cardiovascular system: Pollutants cause narrowing of arteries, increased blood pressure, plaque formation, heart rhythm abnormalities and risk of heart attack.
- Brain and nervous system: Particles can trigger neuroinflammation, increase risk of stroke, dementia, cognitive decline and mood disorders.
- Reproductive system: Studies indicate that exposure to air pollution reduces sperm quality, increases infertility, and affects fetal growth and development.
- Kidneys and liver: Pollutants have been associated with kidney disease, liver damage, and metabolic disorders like diabetes.
In effect, Air Pollution Organ Damage is not an “additional risk”- it is already woven into the fabric of life for many in high-pollution zones.
heart, brain, kidneys, reproductive system & more
Heart and cardiovascular system
The risk increase is evident. A study shows that “even a slight spike in PM2.5 can increase risk of heart attack by 2.5 per cent the very same day”. Another analysis emphasised that particulate matter leads to plaque formation, narrowed arteries and elevated blood pressure, all contributing to heart attacks and strokes. These reflect core components of Air Pollution Organ Damage.
Brain and cognitive health
Air pollution’s effects on the brain are only recently being appreciated. As one expert noted: “It’s harming your brain, too … how toxic air affects your heart, brain, and children’s growth.” The implications: increased risk of dementia, reduced cognitive ability in children, mood disorders, memory issues. Those are major pieces of the Air Pollution Organ Damage puzzle.
Kidneys, liver and metabolic health
Studies based in India reveal strong associations between polluted air and hypertension, diabetes, anaemia and lipid disorders. Once again, Air Pollution Organ Damage extends beyond visible symptoms to metabolic and organ-level dysfunction.
Reproductive system and children’s health
Children and pregnant women face a double jeopardy. Exposure can lead to reduced lung growth, developmental delays, lower IQ, pre-term birth, intra-uterine growth retardation and congenital abnormalities. For adults too—infertility, reduced sperm count and reproductive disorders are increasingly linked to poor air quality—part of the broader sweep of Air Pollution Organ Damage.
Other organs and systems
Beyond the major ones above: chronic exposure affects immune system regulation, skin barrier function, and even eyes (allied organs). One article states- “Even animals… pollutant entry can reach skin, brain, kidneys, liver and more.”
Who is most vulnerable to Air Pollution Organ Damage
Children and teenagers
Because lungs, brains and bodies are still developing, children absorb more pollutants relative to body size, breathe faster, and thus suffer greater long-term consequences.
Elderly and those with pre-existing conditions
Those with heart disease, lung ailments (COPD/asthma), diabetes or weakened immunity are at higher risk of organ damage from pollution.
Pregnant women and unborn children
The “fetal programming” effect means prenatal exposure leads to future health burdens: childhood disorders, developmental delays, chronic conditions.
General population in high-pollution zones
Crucially: even “healthy” adults are not immune. Short-term exposure can trigger cardiovascular or neurological effects.
In short, when we consider Air Pollution Organ Damage, the vulnerable populations are broad, and the risk extends to virtually everyone exposed to long-term or high-level pollution.
Real-life data from Delhi-NCR making the crisis visible
AQI and smog levels
In Delhi and NCR, the onset of winter invariably brings a surge in AQI values into the “poor” to “severe” range. Local data show weekly AQI sometimes hitting 350–400 in certain localities. (“Every year… AQI worsens with winter.”)
Mortality linked to air pollution
Recent analysis: In 2023, nearly 15 % of all deaths in Delhi were linked to ambient air pollution.
Evidence of organ damage beyond lungs
- A Times of India article reported: “Exposure to even one hour of toxic smog can… trigger kidney, liver, fertility problems.”
- An Indian Express piece: “A slight spike in PM2.5 can increase risk of heart attack by 2.5 % the same day.”
- NDTV article: “Ultrafine particles can enter the bloodstream, reaching organs such as the heart, brain and kidneys.”
Together these show how Air Pollution Organ Damage is already operating in the field—not just as theory but as data-driven reality.
How to protect yourself from Air Pollution
Since Air Pollution Organ Damage spans across organs, the protective strategy must be multi-layered.
Indoor protection
- Use air purifiers, especially in bedrooms and living rooms, although they don’t offer complete protection.
- During severe pollution days, minimize opening windows; keep recirculate mode turned on in ACs.
Outdoors and behavioural changes
- Wear N95/N99 masks correctly when stepping out during high AQI days. Experts emphasise correct fit.
- Avoid exercise/outdoor activities early morning or late evening during smog peaks.
Health-oriented lifestyle
- A diet rich in antioxidants helps combat oxidative stress triggered by pollutants.
- Stay hydrated, sleep well, avoid smoking or other pollutants.
- For pregnant women or families with children: monitor air quality, avoid exposure peaks, follow paediatric/adult physician guidance.
Community & systemic awareness
- Keep track of local AQI dashboards. In Delhi: visit or similar sites.
- Be aware of susceptible times: crop-burning season (post-monsoon/winter), temperature inversions, low wind.
While personal measures are important, they are only part of the solution—because the root cause is ambient.
The policy and systemic gap
Inadequate recognition of organ-wide damage
Despite mounting evidence, policies still emphasise respiratory illness. The term Air Pollution Organ Damage is rarely used in official discourse. Studies show that while respiratory and cardiovascular links are known, metabolic, renal and neurological effects are less addressed.
Enforcement and real-time action lag
High-pollution episodes follow stubble-burning, vehicular emissions, industrial output and urban dust. While there are curbs (podies, fire-cracker bans), systemic enforcement in high-pollution zones remains weak.
Healthcare system readiness
Many physicians are trained to treat lung or heart issues, but aren’t routinely linking them to ambient air pollution as underlying cause. Research shows health and environment departments operate in silos.
Public awareness & shifting narrative
Popular perception still limits pollution damage to lungs. Framing it as Air Pollution Organ Damage—spanning brain, heart, fertility, kidneys—could mobilise stronger public and political action.
The cost of inaction
Reduced life expectancy, increased burden of chronic disease, greater healthcare costs and productivity loss all flow from unchecked Air Pollution Organ Damage. Recognising and acting on it is not optional—it’s imperative.
Air Pollution Organ Damage is not a remote future scenario—it is playing out now among millions, particularly in regions like Delhi-NCR. What began as visible lung-disease has widened into a systemic assault on our bodies. From hearts and brains to kidneys and reproductive systems, the evidence is clear: the air we breathe matters.
Andhra Pradesh
pregnant-weightlifting-145kg-feat-redefines-strength-

Contents
Andhra Pradesh, Oct.31,2025:Pregnant weightlifting has entered the public consciousness in a dramatic way, as one woman’s extraordinary feat pushes the boundaries of strength, motherhood and societal expectation. The story of this lift—145 kg at seven months’ pregnancy—sparks both awe and debate- what happens when pregnancy meets serious athletic performance-
Who is the athlete behind the lift
The central figure is Sonika Yadav, a constable in the Delhi Police, who competed in the All India Police Weightlifting Cluster 2025‑26 held in Andhra Pradesh.
Her back-story adds layers to this achievement-
- She joined the Delhi Police in 2014 and has been active in sports, including kabaddi and powerlifting.
- In 2022 she began a more rigorous fitness journey when she was considerably overweight and struggling with lifestyle diseases. She shifted into weightlifting training.
- In 2023 she won gold in a state deadlift competition and then, when she realised she was pregnant, instead of stepping back she chose to continue with medical supervision.
Her motivation: to break the narrative that pregnancy equals pause; she has said she wanted to show that motherhood and athletic ambition can go hand-in-hand.
145 kg and a bronze medal
During the competition, Sonika lifted a total of 145 kg in the deadlift portion, while being seven months pregnant.
Specifically-
- She first performed 125 kg in squats, 80 kg in bench-press, then moved on to a planned 135 kg deadlift but raised it to 145 kg.
- She secured a bronze medal in the 84 kg category at the All India Police Weightlifting Cluster.
- In her own words: she didn’t want pregnancy to be seen as a limitation, and she thought: “If they [other pregnant athletes] can do this, why can’t I?”
This event has been widely shared on social media and covered by major news outlets, capturing public attention for both its positive and contentious implications.
Public reaction
The achievement generated a two-fold reaction: celebration and concern.
The celebration
Many applauded the boldness and determination of Sonika — a woman in uniform, yet also a mother and soon-to-be mother, showing strength in every sense. Her message: pregnancy isn’t a weakness. Her story inspired many who feel sidelined by cultural expectations.
The alarm
On the flip side, commentators raised questions about safety. Some described the act as “risky” or “irresponsible”, warning that heavy lifting while pregnant could endanger the mother and unborn child. According to one report:
“…questions whether heavy occupational lifting during pregnancy is safe.”
This mix of praise and caution places pregnant weightlifting in a contested zone — between empowerment and risk.
Is pregnant weightlifting safe
What experts say
According to senior obstetrician Dr. Nikhil Datar, each pregnancy is unique-
“Some women with medical clearance and supervision can continue strength-training safely. But this case is special – an athlete with years of training.”
He cautions:
“Heavy occupational lifting or high-intensity sets are not generally recommended.”
Key considerations
When assessing pregnant weightlifting the following matter-
- The woman’s baseline fitness level and training history (in this case, years of powerlifting).
- Medical clearance and ongoing monitoring. Sonika reported she consulted her doctor and continued under supervision.
- The intensity and load: what constitutes “heavy” weight differs based on individual capacity.
- The stage of pregnancy: Seven months is advanced, and physiological changes (hormones, joint laxity, heart rate, oxygen demands) become significant.
- The difference between recreational strength training and competitive heavy lifts in a setting.
Thus: pregnant weightlifting can be done safely under certain conditions — but what Sonika did is exceptional, not standard.
Guidelines for strength training during pregnancy
Given the above, what can pregnant individuals consider if they want to stay active through strength training? Below are general guidelines (not personalised advice)-
Consult your healthcare provider
Always begin with a prenatal check-up and get a plan tailored to your health, fitness history, and pregnancy stage.
Choose appropriate load and intensity
- Focus on moderate resistance: safe strength work rather than maximal lifts.
- Avoid sudden heavy loads or maximal single-reps unless under expert supervision.
- For example: walking, body-weight strength, supervised machines may be preferable.
Monitor your body’s signals
Be attentive to-
- Pelvic, abdominal or back pain.
- Dizziness or breathlessness.
- Swelling or reduced foetal movements.
- Joint instability (due to pregnancy hormones).
Prioritise position, posture and stability
- Use machines or supported benches rather than unstable loads.
- Avoid lying flat on back after first trimester if instructed by physician.
- Maintain core engagement, minimise valsalva (holding breath during lift).
Avoid extremes
High-intensity or heavy occupational lifting (e.g., very heavy deadlifts) carry higher risk and require expert monitoring. As Dr. Datar notes, Sonika’s case is not the baseline.
Shift goals from “performance” to “health and wellness”
During pregnancy, the goal can shift: maintain strength, promote circulation, assist recovery and mood — rather than chasing personal records.
For further reading on exercise in pregnancy see the NHS guidance or the American College of Obstetricians and Gynaecologists (ACOG) resources.
The bigger narrative
Beyond the technicalities, Sonika’s story speaks to bigger themes surrounding pregnant weightlifting and women’s roles in society.
Challenging the “pause” narrative
In many societies, pregnancy is framed as a period of rest, withdrawal or at least drastically reduced activity. Sonika turned that on its head-
“I didn’t want pregnancy to be seen as a limitation.”
Role-modelling strength for women
Her lift sends a message: a woman can be a mother, a professional (police officer) and an athlete — roles often siloed by expectation. The wider public reaction (both cheers and criticisms) spotlights how unusual this is still considered.
A conversation starter on risk, agency and support
While not everyone should attempt what she did, her choice raises the question: how much agency do pregnant women have in shaping their bodies, ambitions and physical lives? And how many feel constrained by societal expectations of motherhood?
What her story signals for the future of sport
Sporting bodies have begun adapting for pregnant athletes (e.g., in track and field, team sports). The question of pregnant weightlifting invites reflection on how training protocols, coaching, athlete-care and cultural practices might evolve.
What this means for women in sport
Pregnant weightlifting may sound provocative, even controversial—but the story of Sonika Yadav shows that with preparation, guidance, and experience, boundaries can be pushed.
What we learn-
- Fitness and ambition need not stop during pregnancy — but must be recalibrated.
- Every pregnancy differs; what’s feasible for one woman isn’t for another.
- Societal narratives around pregnancy often restrict rather than empower; stories like this challenge them.
- Fitness professionals, doctors and athletes must collaborate more deeply to develop safe pathways for pregnant athletes.
Caution remains important. This is not a call for every pregnant woman to take up heavy deadlifts. Instead, it signals an evolving understanding of what pregnancy can look like in terms of physicality and agency.
Breaking News
Mental health crisis in India youth with new data- from soaring anxiety & depression to the hidden pressure of social media-
Contents
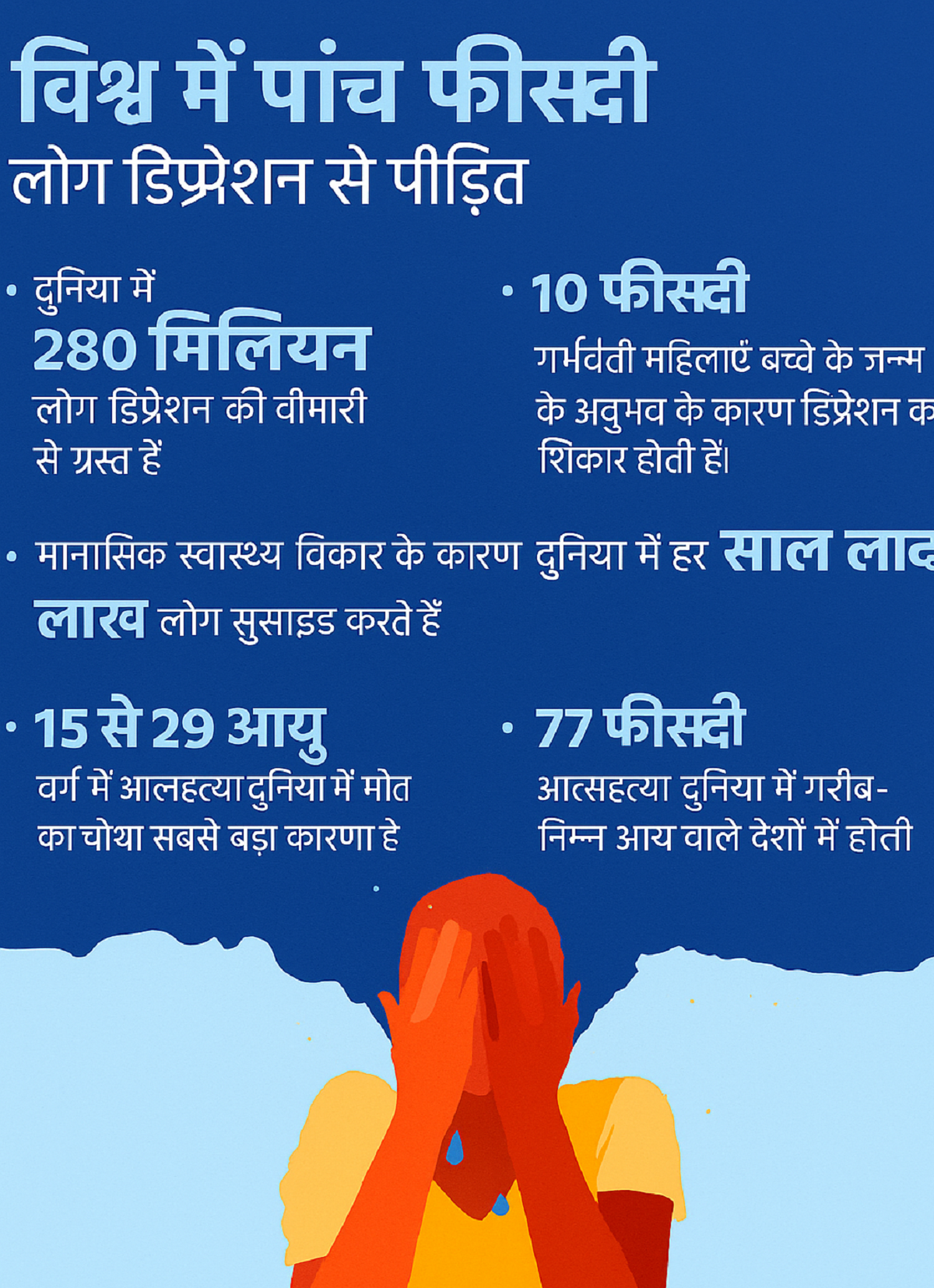
New Delhi, Oct.14,2025:Mental health crisis in India youth is no longer a whisper from the fringes—it has become a loud alarm that demands attention. Across urban and rural regions, among students and young professionals, anxiety, depression, emotional distress, and suicidal thoughts are rising sharply. This article unpacks the data, digs into the causes, and highlights what can be done before the crisis deepens further-
Alarming statistics- how widespread is the issue
Study in Tier-1 cities
A recent study conducted by SRM University AP, Amaravati, published in the Asian Journal of Psychiatry, surveyed 1,628 students (aged 18–29) across eight major Indian cities (Delhi, Mumbai, Bengaluru, Chennai, Hyderabad, Pune, Ahmedabad, Kolkata). Findings include:
- Nearly 70% of students reported moderate to high anxiety.
- About 60% showed signs of depression.
- Over 70% felt emotionally distressed.
- 65% struggled to regulate behaviour or emotions.
Other relevant data
- Among adolescents in Telangana and Karnataka (ages 10-18), over 60% reported sleep difficulties; 70% reported problems focusing in class.
- In India’s workforce and academic settings, nearly 75% of high school students sleep fewer than 7 hours due to late-night social media use; many feel career uncertainty.
- UNICEF reports indicate only 41% of young people in India believe it’s good to seek help for mental health problems, compared to ~83% in many other countries.
- Treatment gap and professional shortage
- India has about 0.75 psychiatrists per 100,000 people, far below WHO recommendations.
- Treatment gap for mental disorders is estimated between 70% to 92%, depending on region and disorder.
These numbers show that mental health crisis in India youth is wide, serious, and multi-dimensional.
Case studies- when social media becomes a trigger
While data gives scale, real stories show the human toll. They mirror many of the trends uncovered by recent studies and add urgency to the need for prevention.
- Case 1: In Raipur (Chhattisgarh), a 22-year-old man who made reels and videos felt despair when his recent posts didn’t get many views. He increasingly isolated himself and one day injured himself via cutting his wrist. Family intervened just in time and got medical help.
- Case 2: In Bhopal, a 23-year-old woman preparing for competitive exams felt immense pressure, loneliness, and repeated failures. She attempted suicide when she felt she had no outlet—this, despite being academically good. Intervention came in time, with help from family and mental health professionals.
These stories underline how external validation (likes, views, status), social isolation, peer comparison, and academic pressure can interact with vulnerabilities, causing crises.
pressure, lifestyle, pandemic impact
Academic, peer & social media pressure
Students cite overwhelming competition, expected academic success, job prospects, etc. Social media amplifies peer pressure: lifestyle comparisons, social status, likes/views become measures of self-worth. Studies show high social media usage correlates with anxiety, sleep issues, and emotional distress.
Lifestyle changes and lack of physical activity
In many cases, children and young adults have decreased physical activity, increased screen time, poor sleep habits, and irregular routines. These contribute to emotional instability, mood disorders, and even physical health issues. This is in line with child psychiatry experts’ observations. (Your original cases about media, gaming addiction, lack of physical activity illustrate this.)
Pandemic after-effects and isolation
COVID-19 lockdowns, disruptions in schooling / college, increased remote/online interactions have caused prolonged isolation. Reports show that youth aged 18-24 were among the worst affected in their mental health scores post-pandemic.
Lack of early support, stigma & awareness
Although awareness has increased, many young people do not recognize early signs. Many are reluctant to seek help due to fear of being judged or due to lack of access. UNICEF data shows low rates of belief in seeking mental health support in India relative to other countries.
physical and psychological links
The mental health crisis in India youth doesn’t only affect emotions—it has broader health and social consequences.
- Physical health risks: Conditions like hypertension, diabetes, heart disease are rising in tandem with mental stress. Stress hormones affect sleep, diet, and bodily systems. In your source data, psychiatric experts note links between mental distress and these physical disorders.
- Emotional regulation & behaviour problems: Youth may have difficulty managing mood, behaviour, impulsivity. Increased substance use, self-harm, or suicidal ideation may follow, especially when pressure or rejection (e.g. from social media) is perceived.
- Academic, social, relational impact: Decline in performance, drop in self-esteem, withdrawal from friends/family, breakdowns in relationships. As in the cases you describe.
- Long-term risk: Early mental health conditions often predict recurrent problems, even in later adulthood. Unaddressed depression or anxiety may lead to chronic illness, lower life satisfaction.
studies, support systems, campaigners
University & survey reports
- The SRM University AP study (1,628 students) as mentioned above.
- Studies on adolescent girls’ mental health, including awareness programmes in remote or rural areas (e.g. Assam, Telangana).
Helplines & tele-mental health
- Tele-MANAS in Karnataka has received over 65,000 calls since its launch in 2022, supporting young people in crises.
- New mental health helpdesk for medical students in Telangana (T-JUDA) to offer peer support, counselling.
Government & policy efforts
- Economic Survey 2024-25 underscores need for preventive mental health education, digital services, workplace policies.
- UNICEF’s “Mental Well-being for Young People” approach that emphasizes integrated services, early detection, reducing stigma.
Community, grassroots action
- Peer-led programmes, student support groups, awareness in schools.
- Workshops and community health clinics in tribal or rural areas improving access (e.g. Gadchiroli study).
What needs to change-solutions and early interventions
To address the mental health crisis in India youth, multiple coordinated steps are essential:
Early identification & screening
- Integrate mental health screening in schools, colleges. Trained counsellors should observe signs: sleep problems, withdrawn behaviour, changes in mood or performance.
- Use validated tools, possibly AI/technology-assisted where feasible, especially after the rise in digital mental health studies.
Awareness & destigmatization
- Reduce shame attached to mental illness. Public campaigns, peer testimonials, role models speaking out.
- Educate parents, teachers, employers about what mental illness may look like, that it can be treated, and help exists.
Improve access to professional care
- Increase number of psychiatrists, psychologists, psychiatric social workers. WHO recommendation is higher than current ratio.
- Enhance tele-mental health services: helplines like Tele-MANAS, online counselling.
Support systems in institutions
- Schools and colleges should have counselling centres, peer support cells. Emotional support should be part of curriculum.
- Employers should build policies allowing mental health days, wellbeing programs, reduce burnout.
Healthy lifestyle & digital balance
- Promote physical activity, sleep hygiene, limits on screen time.
- Teach young people digital literacy: how social media works, how comparison and algorithms can amplify distress.
turning awareness into action
The mental health crisis in India youth is a reality. It’s visible in statistics, in heartbreaking case studies, and in every city and rural area where young people suffer in silence. But there is also hope. Awareness is rising. Institutions, researchers, policy makers, and community actors are stepping in.
Breaking News
Excess Rice and Roti Consumption Linked to Rising Diabetes Risk in India – ICMR Study 2025-

Contents
New Delhi, Oct.10,2025:The ICMR Study 2025 has issued a stark warning to Indian households: overconsumption of rice and roti — staples of the Indian diet — could be driving an alarming rise in diabetes, obesity, and metabolic disorders across the country. Conducted by the Indian Council of Medical Research (ICMR) in collaboration with the Madras Diabetes Research Foundation (MDRF), this large-scale study offers deep insight into how India’s eating patterns are affecting public health-
According to the research, 62% of India’s daily energy intake comes from carbohydrates, primarily white rice, wheat, and processed grains. These foods, though culturally integral, are significantly contributing to poor metabolic health outcomes.
High Carbohydrate Dependence in Indian Diets
The ICMR Study 2025 examined food consumption habits across 30 states and union territories, involving adults aged 20 years and above. The results reveal a concerning pattern — most Indians rely heavily on refined carbohydrates while consuming inadequate protein and fibre.
The data showed-
- Carbohydrates: 62.3% of total daily energy
- Fats: 25.2%
- Proteins: only 12%
The study also highlighted that processed grains contribute 28.5% and whole grains contribute 16.2% to total carbohydrate intake. Such an imbalance between nutrient groups makes Indians highly vulnerable to metabolic conditions like Type 2 diabetes and obesity.
Diabetes and Obesity Connection Explained
Published in Nature Medicine, the ICMR study notes that individuals consuming the highest levels of carbohydrates are 30% more likely to develop diabetes compared to those on low-carb diets. Additionally, the risks of general obesity increase by 22% and abdominal fat accumulation by 15%.
India already accounts for nearly one-fourth of the world’s diabetes cases, a number that continues to grow faster than in most countries. The report attributes this to excessive carbohydrate consumption, coupled with a sedentary lifestyle.
Processed vs Whole Grains – The Hidden Truth
While traditional wisdom suggests that whole grains like millets or brown rice are healthier alternatives, the ICMR Study 2025 warns that merely switching from processed to whole grains may not be enough.
The research indicates that even unprocessed wheat or millet flours do not significantly reduce diabetes risk when consumed in excess. This is because high carbohydrate intake — regardless of its source — leads to elevated blood sugar and insulin resistance over time.
Nutrition experts emphasize balancing grains with protein-rich foods and fibre, which help slow down sugar absorption.
What Experts Are Saying About the Findings
Dr. Vibhuti Rastogi, Senior Dietitian at the Institute of Human Behaviour and Allied Sciences (IHBAS), told that Indian diets are indeed “too carb-heavy and too low in protein,” which accelerates the onset of lifestyle diseases.
“Both refined and simple carbohydrates, such as sugar, can increase diabetes risk. But when combined with low protein intake, the damage happens faster,” Dr. Rastogi explained.
Similarly, Nazneen Hussain, Head Dietitian at Dietetics for Nutrify Today (Mumbai), highlighted that the type of carbohydrate also matters.
“If you eat rotis made from refined flour, they’re almost as bad as polished rice. Choose coarse or fibre-rich flour to slow blood sugar spikes,” she advised.
She also noted that brown rice or unpolished small-grain rice are healthier alternatives but must be eaten in moderation and with fibre, dal, or vegetables for balance.
Regional Differences in Health Risks
The study found striking regional variations in obesity and metabolic disease rates:
- North India: 54% overweight, 37% obese, and 48% had abdominal obesity
- East India: Showed the best metabolic health indicators nationwide
- Overall: 83% of participants showed at least one metabolic risk factor
Additionally, 27% of adults nationwide suffer from hypertension, a condition often linked with excess carbohydrate and sodium intake. Interestingly, these trends showed little regional difference — indicating a nationwide dietary imbalance.
How to Reduce Carbohydrate-Related Health Risks
Experts recommend gradual dietary transitions rather than drastic eliminations. Here’s how to make daily Indian meals healthier, based on ICMR’s recommendations:
- Reduce refined grains: Replace white rice with brown rice, millets, or quinoa.
- Increase protein intake: Add dals, paneer, eggs, tofu, or lean meats.
- Add healthy fats: Use nuts, seeds, and olive or mustard oil instead of saturated fats.
- Control portion sizes: Especially for rice and roti at dinner.
- Include fibre-rich foods: Vegetables, salads, and legumes improve digestion and metabolism.
Lifestyle Changes to Control Diabetes Risk
Beyond diet, the ICMR Study 2025 found that 61% of participants were physically inactive. Regular exercise can reduce Type 2 diabetes risk by up to 50%, according to global health data.
Recommended lifestyle changes–
- Walk or exercise at least 30 minutes daily
- Practice yoga or light resistance training
- Limit sugary drinks and late-night snacking
- Sleep 7–8 hours daily
- Get routine blood sugar check-ups, especially if above 30
Combining these habits with balanced nutrition can reverse early-stage metabolic disorders, experts say.
The Way Forward for a Healthier India
The ICMR Study 2025 is a wake-up call for India’s food culture. While rice and roti remain dietary staples, overreliance on these high-carb foods is quietly eroding public health. With nearly 83% of adults showing metabolic risks, the nation must rethink its traditional plate.
Nutrition experts unanimously agree — moderation, balance, and movement are key. By incorporating more proteins, healthy fats, and fibre, alongside regular physical activity, India can curb the rising tide of diabetes and obesity.

 Credent TV2 weeks ago
Credent TV2 weeks agoUKG Graduation Ceremony at St. Xavier’s School Nevta: 7 Heartwarming & Inspiring Moments from a Grand Spiritual Celebration

 Art2 weeks ago
Art2 weeks agoIndian Art History Congress 2026: 5 Powerful Insights from Dr. Renu Shahi’s Groundbreaking Satire Art Research in Bengaluru

 Breaking News4 days ago
Breaking News4 days agoUGC Act 2026: 5 Powerful Demands Raised in Rajasthan to End Campus Discrimination

 Breaking News2 days ago
Breaking News2 days agoInternational Women’s Day 2026: 7 Powerful Highlights from the Inspiring Jaipur Celebration by Dr. Ambedkar Memorial Welfare Society



















